As health care has become increasingly technology driven and demanding, there has been a growing need to develop health professionals who can work at an advanced level. The introduction of advanced clinical practitioners (ACPs) has led to a blended workforce within the medical team. This is particularly important in areas such as critical care. Continuous professional development for practitioners is essential to consolidate learning, maintain competency and further develop clinical examination and decision-making skills. Although hyponatraemia is commonplace, affecting around 40% of patients in critical care and 30% of inpatients (Friedman and Cirulli, 2013), there is a paucity of literature on this subject within nursing journals. Therefore, this clinical review will focus on hyponatraemia, its diagnosis, and treatment, and is particularly aimed at ACPs working in critical care.
Hyponatraemia
The recognised normal range for serum sodium concentration (SNa) in adults is accepted as 135-145 millimoles per litre (mmol/litre). Hyponatraemia is more commonly an excess of total body water rather than sodium deficiency, being defined as an SNa of less than 135 mmol/litre. It is classified into mild (130-134 mmol/litre), moderate (125-129 mmol/litre) or severe hyponatraemia (an SNa below 125 mmol/litre). Severe hyponatraemia is prevalent in 2-3% of patients (Winzeler et al, 2016; National Institute for Health and Care Excellence (NICE), 2020).
Within critical care, arterial blood gas (ABG) analyses are performed frequently, identifying altered electrolyte results early and allowing appropriate treatment. However, with point-of-care testing, the ACP should interpret the results with caution, requesting a formal laboratory report to support their clinical decision-making. Frequent ABG results can guide the trend of improvement or decline (Kim et al, 2016).
Mortality and comorbidities
Lopez-Ruiz and Niven (2017) defined hyponatraemia as a consequence of a water–electrolyte imbalance rather than an individual disease. It is associated with poor outcomes, including increased mortality, prolonged hospital admission, cognitive impairment and increased morbidity due to falls and fractures (Lu et al, 2020). Lu et al (2020) found a 55% increase in mortality in patients with hyponatraemia. Corona et al (2015) also established a relationship between hyponatraemia and mortality, involving diverse comorbidities such as pneumonia, heart failure, cirrhosis, malignancy and myocardial infarction. Mortality rates increase when untreated hyponatraemia worsens. However, Chawla et al (2011) considered the increased mortality rates as a marker of underlying disease severity rather than a direct consequence of hyponatraemia. Winzeler et al (2016) confirmed this as they determined mortality was influenced by comorbidities; yet Gankam-Kengne et al (2013) identified hyponatraemia as being independently associated with increased mortality.
It is recognised that an acute onset of severe hyponatraemia, developing in less that 48 hours, predominantly symptomatic, is life-threatening and considered a medical emergency (Zhang and Li, 2020). Although in the past mild hyponatraemia (SNa 130-134 mmol/litre) has not been considered a concerning finding, Corona et al (2015) demonstrated conflicting evidence and further studies by Nagler et al found a 30% increase in mortality with mild hyponatraemia, as well as longer hospital stays than in patients with normal SNa (Nagler et al, 2014). Seemingly asymptomatic chronic mild hyponatraemia, more common with increasing age, contributes to disturbed cognition and gait disturbances, significantly increasing the risk of falls and fractures and possible critical care admission (Sterns et al, 2013).
Hyponatraemia is particularly common in older people. With the average age of critically ill patients rising, hyponatraemia, often mild and frequently present at critical care admission, is an independent risk factor for poor prognosis (Padhi et al, 2014). Recognised comorbidities and medications associated with causing hyponatraemia, including age-related changes in homeostasis, may aggravate existing, or provoke iatrogenic hyponatraemia (Zhang and Li, 2020). Verbalis et al (2013) reported iatrogenic factors being responsible in 40–75% of hyponatraemia in inpatients. Consequently, a clear understanding of electrolyte disturbance is required to avoid iatrogenic injury (Sterns et al, 2013). With an ageing population the incidence and severity of hyponatraemia is expected to increase. Therefore the ACP is more likely to encounter patients with electrolyte imbalances. Yet despite the incidence and potential severe complications of hyponatraemia, studies appear to show it is often neglected. Consequently, the ACP should perform regular monitoring of SNa within clinical settings, to ensure early detection and correction of hyponatraemia and thus avoid iatrogenic injury (Nagler et al, 2014; Zhang and Li, 2020).
Critically ill patients often amass contributory factors for hyponatraemia, those of impaired electrolyte-free water excretion, administration of hypotonic fluids, multi-organ dysfunction and medications known to influence hyponatraemia (Rafat et al, 2015). Pneumonia is a leading cause of hyponatraemia. Spending prolonged time on mechanical ventilators and patients requiring renal replacement therapy, increasing the overall critical care stay, are also contributory factors for hyponatraemia, increasing morbidity and mortality (Sim et al, 2020). Friedman and Cirulli (2013) emphasised that hyponatraemia is particularly difficult to prevent and treat in critical care.
Symptoms of hyponatraemia
Although symptoms may not be evident with mild hyponatraemia, acute moderate and severe cases may present with non-specific symptoms such as headache, nausea, confusion and malaise. Within critical care, hyponatraemia is difficult to identify as critical illness presents with similar indicators, signifying a wide range of differential diagnoses (Dineen et al, 2017). Periodic ABG monitoring may recognise declining SNa, revealing hyponatraemia. With the assessment of volume status, this may direct the ACP's clinical decision-making towards correct diagnosis and appropriate management, depending on the aetiology and classification of hyponatraemia (Królicka et al, 2020). However, if hyponatraemia is left untreated, SNa levels may further decrease, with more pronounced severe symptoms: vomiting, impaired consciousness and seizures, indicating severe hyponatraemia requiring urgent treatment (Dineen et al, 2017).
Symptoms are more likely to manifest in acute rather than chronic hyponatraemia, even in clinically severe cases, giving rise to the possibility of developing cerebral oedema, raising intracranial pressure and increasing the risk of cerebral herniation, hypoxia and even death (Dineen et al, 2017). Conversely, within the intensive care unit (ICU), or critical care level 3, symptoms may not be apparent to the ACP in mechanically ventilated and sedated patients, as they are unable to communicate deterioration, therefore worsening cerebral oedema may culminate in devastating effects (Lee, 2010).
Neurological complications
Neurological concerns from hyponatraemia are due to osmotic pressures and the capacity of brain cells adapting to fluctuating osmolality and tonicity. Even minimal changes in cerebral cellular volumes may cause significant effects (Gankam-Kengne and Decaux, 2018). In acute hyponatraemia, the risk of cerebral oedema occurs as brain cells have had inadequate time to adapt to the altered intracellular environment, whereas, in chronic hyponatraemia, the risk of acute neurological symptoms is lower as chronic cerebral adaptive mechanisms minimise the risk of cerebral oedema (Dineen et al, 2017). The distinction between acute and chronic onset of hyponatraemia is a subjective timeframe of 48 hours. It is considered that cerebral adaptive mechanisms are established after this period (Gankam-Kengne and Decaux, 2018). However, asymptomatic hyponatraemia, where onset is undetermined, is usually deemed chronic onset, as chronic hyponatraemia is more common (Seay et al, 2020).
Assessment and management
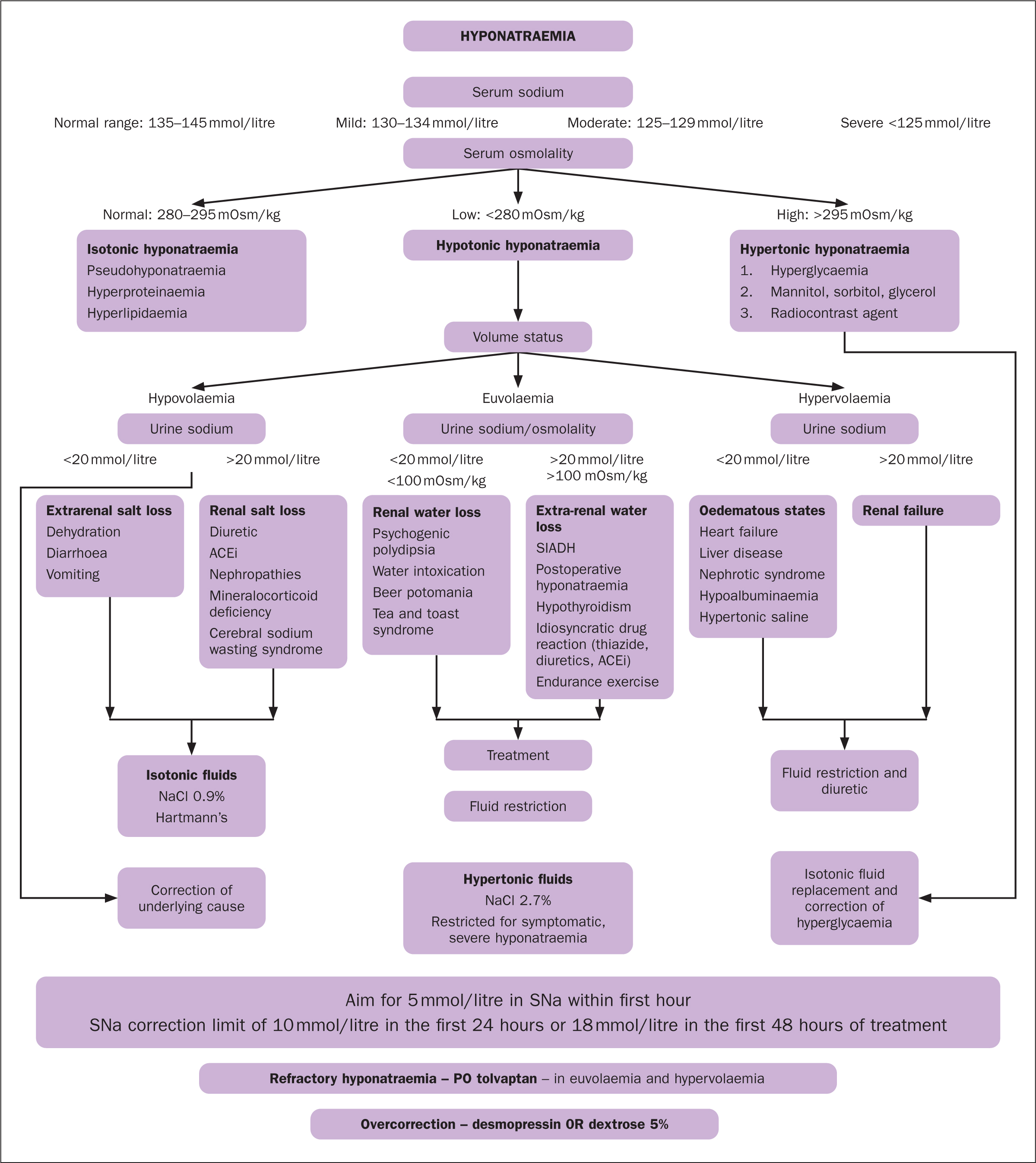
Despite the frequency and severity of complications, evidence suggests management for hyponatraemia is often suboptimal, presenting a challenge for ACPs and all clinicians as aetiology is complex (Nagler et al, 2014). As hyponatraemia is a diverse condition, guidelines standardise and direct management, depending on the cause. However, clinical assessment considers individual cases combined with guidelines for decision-making at the point of care (Spasovski et al, 2014). Local clinical guidelines, usually based on European guidelines (Spasovski et al, 2014), give the ACP a clear structure, providing evidence-based recommendations. Guidelines advocate additional appropriate investigations for serum osmolality, volume status, urinary sodium (UNa) and urinary osmolality (UOSM), to guide differential diagnosis and management (Nagler et al, 2014) (Figure 1). However, Hoorn and Zeiste (2017) found clinicians often misclassify hyponatraemia, as the distinction between volume status, particularly hypovolaemia and euvolaemia, can be challenging, whereas hypervolaemia is obvious. Recent recommendations direct UOSM and UNa as a more accurate marker than volume status assessment, reflecting accurate vasopressin activity and differentiating hyponatraemia further (Dineen et al, 2017).
Hypotonic, isotonic or hypertonic?
The definition of hyponatraemia, with a comparatively greater volume of total body water to that of total body solute, is divided into non-hypotonic (isotonic or hypertonic) and hypotonic (hyponatraemia). Hyponatraemia is further divided in accordance with volume status: hypovolaemia, euvolaemia, hypervolaemia (Królicka et al, 2020) (Figure 1). Hoorn and Zieste (2017) argued that the initial differentiation between hypotonic and non-hypotonic hyponatraemia is significant, as management is different. Hypotonic hyponatraemia generally reflects low osmolality; however, consideration should be given to patients with non-hypotonic hyponatraemia during clinical decision-making (Spasovski et al, 2014). Normal osmolality, consistent with isotonic hyponatraemia, raises suspicion of pseudo-hyponatraemia with pronounced hyperlipidaemia or hyperproteinaemia, culminating in a false low SNa. Conversely, elevated osmolality denotes hypertonic hyponatraemia, observed in hyperglycaemia or excess hypertonic fluid, such as mannitol, often termed translocational, as oncotic pressures influence water intravascularly (Seay et al, 2020). With replenishment of fluids and correction of hyperglycaemia by exogenous insulin, SNa is usually autocorrected (Knott, 2022).
Friedman and Cirulli (2013) stated that hypotonic hyponatraemia is most commonly seen in critical care settings, usually indicating hypervolaemia, where consideration is given to patients with decompensated chronic diseases such as heart failure, liver cirrhosis, renal failure, or euvolaemia, complicated further by syndrome of inappropriate antidiuretic hormone secretion (SIADH) (Seay et al, 2020). Dineen et al (2017) suggested that in decompensated chronic conditions where the mechanism of disease leads to a reduction in mean arterial pressure, decreased renal blood flow, activation of the renin–angiotensin–aldosterone system with sodium and water retention and increased anti-diuretic hormone (ADH) secretion with further subsequent water retention, this leads to hypervolaemia, oedema and dilutional hyponatraemia (Królicka et al, 2020). Liamis et al (2019) noted that treatment options are primarily the management of the underlying condition, which often results in improvement in SNa levels, and diuretic therapy; although diuretics may also exacerbate hyponatraemia (Biswas and Davies, 2007). Friedman and Cirulli (2013) recommend that SIADH, a recognised cause of hyponatraemia in ICU, should be a diagnosis of exclusion and is best managed by elimination of its cause. Numerous causes of SIADH are particular to patients in ICU, including severe infection, acute respiratory failure and medications, which stimulate the release or amplify the effects of ADH (Liamis et al, 2019). Padhi et al (2014) also found hyponatraemia was associated with extended days on mechanical ventilation and therefore longer ICU stays.
Drug- and fluid-induced hyponatraemia
Drugs provoking hyponatraemia make varying pathogenetic alterations to sodium–water homeostasis: diuretic agents, and water homeostasis (SIADH). Numerous drugs fall within the latter category, causing an increase of pituitary secretions and potentiated effects, lowering the threshold of secretion of ADH, also known as vasopressin (Liamis et al, 2019). The ACP should be aware that many medications associated with an increased risk of developing hyponatraemia are commonly used within critical care, such as opiates, diuretics, protein pump inhibitors, various antidepressants and anti-seizure drugs, among other medications (Friedman and Cirulli, 2013). Interestingly, Elhosiny et al (2019) argued that caution is required when prescribing certain antimicrobials, particularly in elderly people, to avoid causing or worsening hyponatraemia. This presents a further challenge for ACPs and all clinicians, since infection also induces hyponatraemia (Liamis et al, 2019).
Vasodilatory shock can result in life-threatening hypotension. Within ICU, exogenous vasopressin, an analogue of ADH, is used to support mean arterial pressure and systemic vascular resistance. However, both beneficial and detrimental effects may be seen (Salazar et al, 2015). Although vasopressin-induced hyponatraemia is infrequent, when used as an adjunct therapy, it may induce fluid retention, instigating subsequent hyponatraemia. Discontinuation can resolve hyponatraemia, highlighting the importance of monitoring electrolytes in clinical settings (Peters et al, 2014).
Sodium-water homeostasis is regulated by ADH release, thirst mechanism and the renin-angiotensin-aldosterone system. Hyponatraemia progresses due to excessive intake or retention of solute-free water, and is rarely due to sodium deficiency (Fogarty and Loughrey, 2017). Critically ill patients are at increased risk of impaired free-water excretion and subsequent hyponatraemia, due to inflammatory, hormonal and metabolic responses stimulated during stress responses to critical illness and major surgery (Finnerty et al, 2013). Endogenous vasopressin secretion increases with hypovolaemia, oedema, stress, pain and surgery, increasing water reabsorption, and potentially worsened by the administration of hypotonic fluids (Lee, 2010; Winata et al, 2019). Postoperative patients, particularly following abdominal surgery, are often initially managed in the high dependency unit (HDU), critical care level 2; Winata et al (2019) highlighted the consequence of choosing inappropriate fluid options when prescribing fluids peri-operatively; hypotonic solutions should be avoided. Furthermore, patients in critical care are frequently prescribed large amounts of intravenous fluids, mainly for resuscitation or replacement purposes (Malbrain et al, 2020). Within critical care settings, supplementary fluid for the reconstitution of medicines for infusions may also potentially increase the risk of electrolyte imbalances further (Lee, 2010).
Although fluid management is essential in the early phase of critical illness to ensure haemodynamic stability, continued inadequate fluid management may precipitate fluid overload and deranged electrolytes (Besen et al, 2015). NICE (2017) advised caution when prescribing fluid, as fluids and electrolyte deficits or excesses may cause harm to patients. Winata et al (2019) considered intravenous fluids comprising key electrolyte requirements in preference to a hypotonic solution, which is associated with greater incidences of postoperative hyponatraemia, and recommended maintaining daily monitoring of electrolytes.
Treatment of hyponatraemia
The severity of symptoms generally determines treatment despite the degree of SNa, although options for mild or moderate symptoms depend on the cause of hyponatraemia, with SNa correcting as the underlying condition improves (Ball et al, 2016). The most cautious treatment is recommended for hypotonic hyponatraemia due to potential complications (Seay et al, 2020). Corona et al (2015) found that correcting hyponatraemia reduced mortality by up to 70% in some cases. Adrogué and Madias (2012) highlighted the challenge of hyponatraemia, suggesting a twofold approach to diagnosis: identifying the cause and rate of onset, if possible, including risks, and a specific management plan based on the classification. The basis of treatment for symptomatic hyponatraemia is the reduction of intracranial pressure by reducing cerebral oedema (Seay et al, 2020). Prompt correction of severe symptomatic hyponatraemia should occur, regardless of chronicity and degree of SNa decline (Gankam-Kengne and Decaux, 2018). However, too rapid correction or over correction of hyponatraemia may risk osmotic demyelination syndrome (ODS), therefore correction with caution is paramount to avoid complications (Ball et al, 2016). Adrogué and Madrias (2012) determined a therapeutic limit rather than a target therapy, giving effective treatment and providing some protection from ODS, which may result after treatment, although the risk is low. Although a rare complication, a suspicion should be raised in patients who develop additional neurological deficits, during or following treatment with hypertonic saline (Patil et al, 2016). Although cerebral oedema is not common in chronic severe hyponatraemia, rapid correction of chronic hyponatraemia is unnecessary as it is associated with ODS and higher mortality (Gankam-Kengne and Decaux, 2018).
The intention of treatment is balancing the risk for morbidity and mortality from cerebral oedema against that of ODS from over rapid correction, by increasing the SNa enough to prevent complications but at a rate that does not risk iatrogenic cerebral injury, although overall management should be directed at resolving the underlying cause, where identified (Fogarty and Loughrey, 2017; Seay et al, 2020). In the absence of severe neurological symptoms, diagnostic assessment and cause-specific treatment is judicious (Spasovski et al, 2014).
Pharmacological treatment
The NICE (2020) clinical knowledge summary and local guidelines support treatment recommended in the European guidelines (Spasovski et al, 2014) for partial rapid early correction of SNa in acute severe symptomatic hyponatraemia, using bolus doses of hypertonic saline, such as 2.7% sodium chloride to reduce life-threatening cerebral oedema (Sterns et al, 2013). The decision to treat hyponatraemia with hypertonic fluid should be restricted to patients with neurological symptoms secondary to severe hyponatraemia and remains the responsibility of a senior clinician (Ball et al, 2016). Garrahy et al (2019) observed that patients receiving bolus dose treatment of hypertonic fluids had more effective correction of SNa than those receiving a continuous infusion. However, consideration should be given to whether therapeutic re-lowering of SNa, using intravenous hypotonic fluid or desmopressin, for rapid over correction, would be more effective, probably due to the speed of correction (Garrahy et al, 2019). Patients treated with hypertonic fluids are often managed in critical care, ensuring frequent monitoring of SNa, and thus safeguarding against rapid over correction (Dineen et al, 2017). With symptomatic hyponatraemia, Gankam-Kengne and Decaux (2018) identified that an increase of 5 mmol/litre in SNa, within the first hour, is sufficient to reduce intracranial pressure to prevent the risk of cerebral herniation. Dineen et al (2017) advocated SNa correction limits of 10 mmol/litre in the first 24 hours; or 18 mmol/litre in the first 48 hours of treatment is deemed safe in clinical practice and is supported by the US and European guidelines (Verbalis et al, 2013; Spasovski et al, 2014). However, if the limit is exceeded or neurological symptoms subside, hypertonic fluids should be discontinued (Ball et al, 2016). With chronic asymptomatic severe hyponatraemia, SNa can be corrected more slowly, with recommended target increases of 4-6 mmol/litre per 24 hours, therefore preventing over correction and iatrogenic injury (Sterns et al, 2013).
Correction of SNa that does not respond to fluid restrictions may benefit from pharmacological treatment. Dineen et al, (2017) advised consideration of vaptans or a vasopressin receptor antagonist, such as tolvaptan, in hypervolaemia hyponatraemia or SIADH. However, other studies have recommended taking precautions against over correction of SNa and subsequent ODS – through frequent monitoring of SNa without fluid restrictions and caution in those with liver dysfunction and kidney disease (Seay et al, 2020).
Conclusion
Hyponatraemia is a common clinical finding within critical care, resulting from various disorders, including infectious diseases, and cardiovascular, renal, hepatic, endocrine, nutritional or metabolic pathologies. Irrespective of the cause, it contributes significantly to mortality and morbidity, and impacts economically on patients and healthcare services (Al Mawed et al, 2018). The complex pathophysiology, including clinical consequences, of hyponatraemia, ranging from asymptomatic presentations to life-threatening conditions, give rise to its challenges. Early recognition of hyponatraemia is a significant factor in reducing the incidence and associated complications. Understanding the presentations and contributing risk factors between acute and chronic hyponatraemia, highlights the different management and prevents further progression of the symptoms. Correction of SNa levels in both acute and chronic hyponatraemia remains key, as hyponatraemia may cause adverse effects on various organs (Sterns et al, 2013).
It is essential that the critical care ACP has a comprehensive knowledge and understanding of hyponatraemia, and remains confident and competent in establishing the severity and appropriate treatment, as well as having an awareness of potential side effects and consequences of incorrect management of the patient. ACPs can support junior doctors rotating into critical care, by guiding appropriate management, highlighting increased risks of hyponatraemia and treatment in critically ill patients. Encouraging clear, concise, and documented communication, particularly to other nurses, as to the targets of increases in SNa, promotes team communication, and effective management of treatment for the patient.
KEY POINTS
- For patients presenting with suspected hyponatraemia, a review of electrolyte levels and a full assessment and investigations is required
- It is important for the advanced clinical practitioner (ACP) to determine whether the condition is acute or chronic, the classification and cause
- Once a diagnosis has been made the correct management can begin, following guidelines
- It is important for the ACP to be aware of the problems associated with too rapid or overcorrection and know what subsequent management should be
- The ACP can educate other staff on hyponatraemia
CPD reflective questions
- What is the normal range of serum sodium and what do you consider as severe hyponatraemia?
- Why is it imperative not to replace sodium too fast in severe hyponatraemia?
- Why is it important to understand the presentations and contributing risk factors between acute and chronic hyponatraemia?


