An oncological emergency is caused by either a cancer or its treatment. It requires rapid intervention to avoid mortality and morbidity. Cancer is the leading cause of death in children up to 14 years of age with the exception of accidents (Public Health England (PHE), 2018). Oncological emergencies can present at the initial diagnosis but also may occur due to cancer progression, recurrence, or as a side-effect of cancer treatment. This article discusses the recognition and acute management of the most common oncological emergencies. These include neutropenic sepsis, hyperleukocytosis, raised intracranial pressure, tumour lysis syndrome (TLS) and superior mediastinal syndrome, which are likely to be encountered by nurses working in different non-specialist settings. Two illustrative case studies are included to demonstrate some of the challenges that nurses may encounter in clinical practice.
Epidemiology
In the UK each year, around 1900 new cases of childhood (0-14 years) cancers are diagnosed (Children with Cancer UK, 2021). The most common are:
- Leukaemia: 30%
- Brain and spinal tumours: 26%
- Lymphomas: 11%
- Soft tissue tumours: 6%.
In the UK, around 240 children die from cancer each year (Children with Cancer UK, 2021). In England, this accounts for 6% of all deaths in children aged 0-14 years (PHE, 2018). Excluding infants, deaths from cancer account for an even greater proportion (20%) of total deaths; in this age group, cancer is the leading cause of death from a single disease entity (PHE, 2018). The National Institute for Health and Care Excellence (NICE)-accredited Diagnosis of Brain Tumours in Children guideline (The Brain Tumour Charity, 2017; 2018) has helped to reduce the time to diagnosis of brain tumours from symptom onset from just over 13 weeks down to the current 6.5 weeks. Improving the speed of diagnosis may potentially result in a significant impact on the prognosis of cancers.
Clinical presentations
Oncological emergencies may present unexpectedly and it is important to remain aware of how to identify and initiate urgent management for these conditions. This is outlined in Table 1.
Table 1. Summary of oncological emergencies and acute management
| Condition | Presentation | Investigations | Management |
|---|---|---|---|
| Neutropenic sepsis (National Institute for Health and Care Excellence, 2012; UK Sepsis Trust, 2021) |
|
|
|
| Hyperleukocytosis (Seth and Bhat, 2011; Giammarco et al, 2017) |
|
|
|
| Brain tumours presenting with raised intracranial pressure (Wilne et al, 2012) |
|
|
|
| Tumour lysis syndrome (Jones et al, 2015; Mirrakhimov et al, 2015) |
|
|
|
| Superior mediastinal syndrome (Seth and Bhat, 2011) |
|
|
|
Key: ABCDE=Airway, Breathing, Circulation, Disability, Exposure; CT=computed tomography; ECG=electrocardiogram; IV=intravenous; MRI=magnetic resonance imaging; PICU=paediatric intensive care unit
Neutropenic sepsis
Neutropenic sepsis is seen when an infection occurs concurrently with a low neutrophil count. It occurs most commonly as a complication of cancer treatments, particularly chemotherapy, but it may be due to cancer itself (de Naurois et al, 2010). Neutropenic sepsis is potentially life threatening as the immune response is diminished and thus the child is very vulnerable to overwhelming infection and sepsis (NICE, 2012).
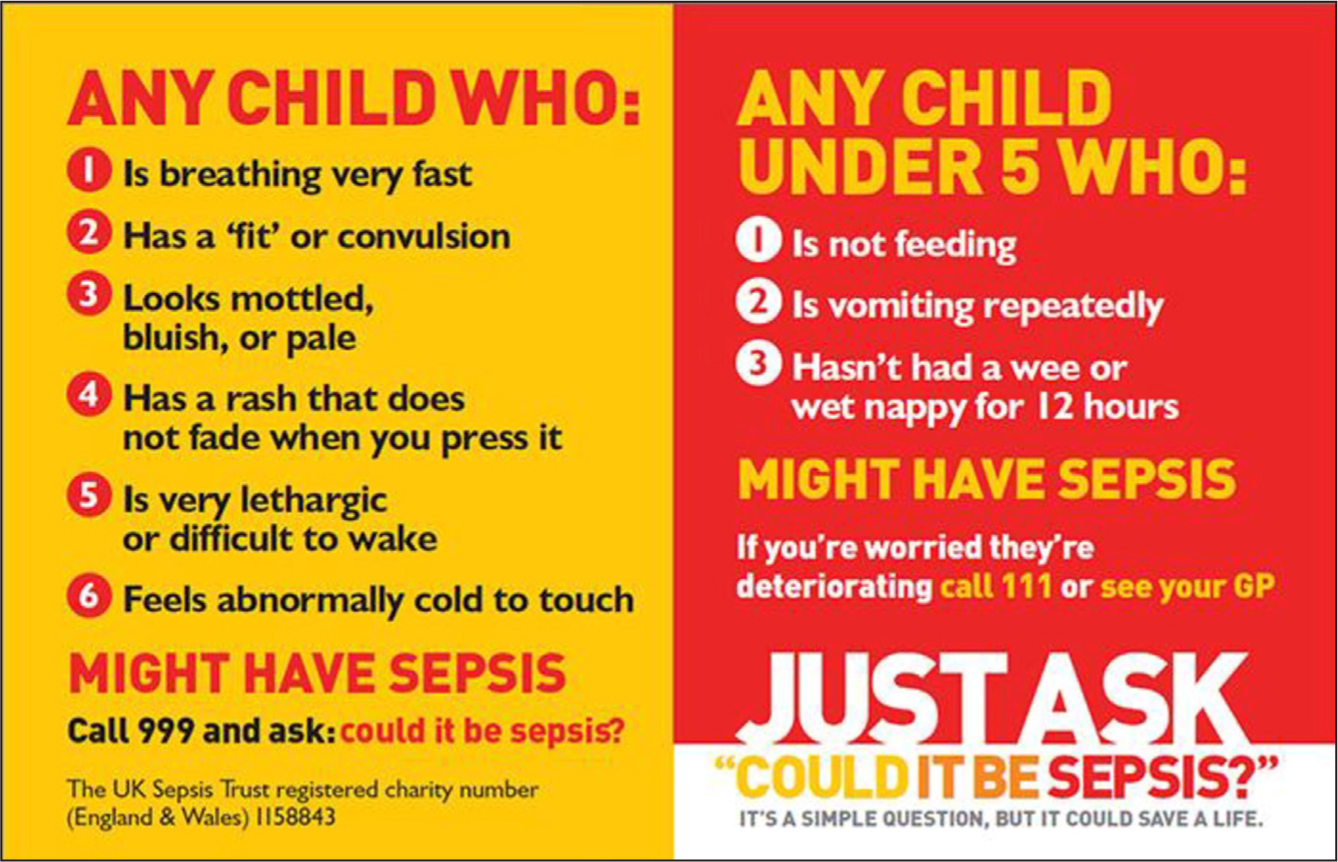
The ‘Paediatric Sepsis Symptom Card’ (UK Sepsis Trust, 2021) (Figure 1) provides useful guidance on the most common symptoms seen in children and may be used in conjunction with the NICE guidance (2012) when assessing a child for suspected neutropenic sepsis.
Hyperleukocytosis and leukostasis
Hyperleukocytosis is defined by ‘a white blood cell count of 50 x 109/litre or 100 x 109/litre’ and can be the initial presentation or a complication of acute leukaemia (acute lymphoblastic leukaemia (ALL) or acute myeloid leukaemia (AML)) (Giammarco et al, 2017). Leukostasis is a pathologic diagnosis in which white cell plugs are seen in the microvasculature and is typically diagnosed empirically when a patient with leukaemia and hyperleukocytosis presents with respiratory or neurological distress. Prompt treatment is indicated because, if left untreated, there is approximately 20-40% mortality within 1 week (Bruserud et al, 2013)
Brain tumours presenting with raised intracranial pressure
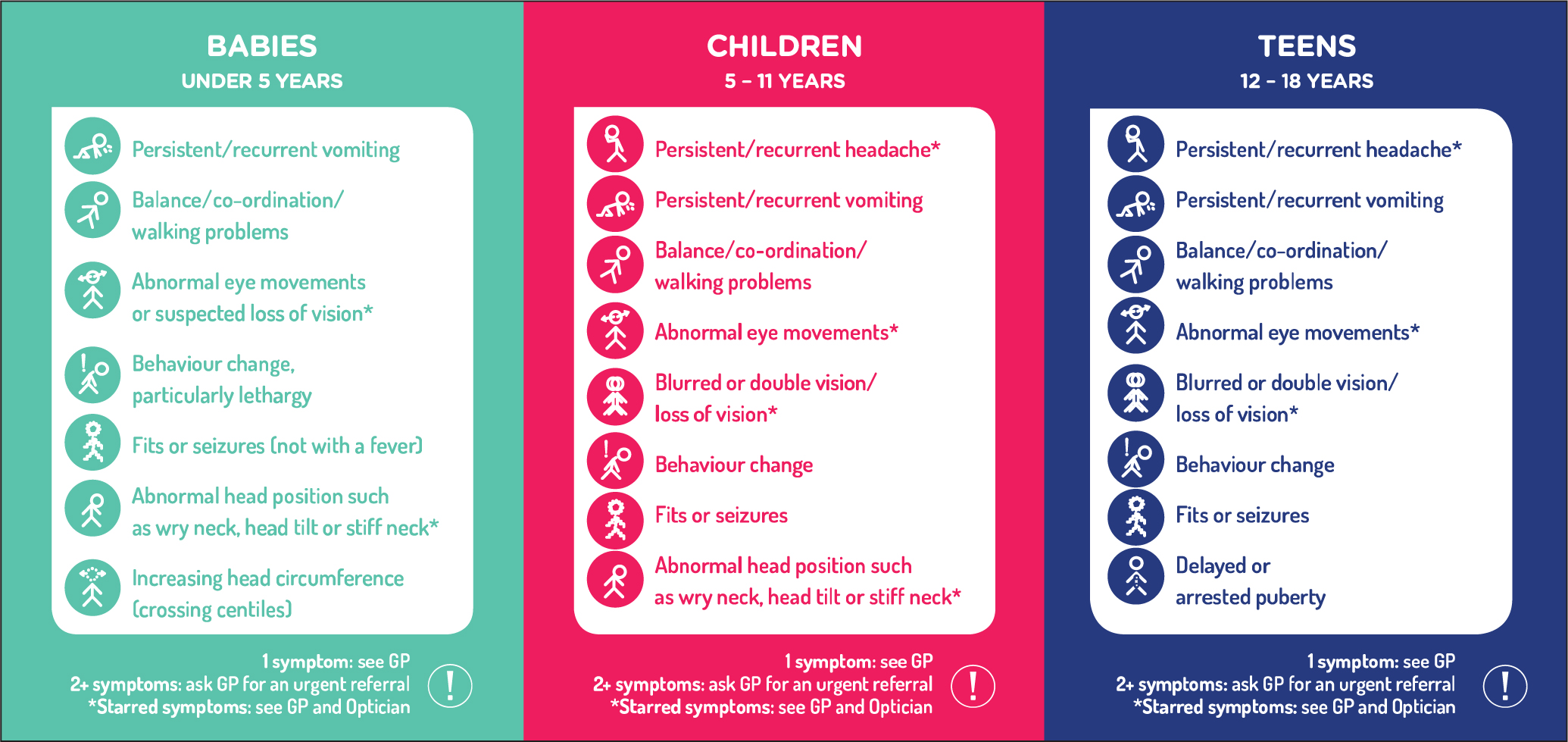
Raised intracranial pressure (ICP) may result from a number of conditions; brain tumours are an important diagnosis to consider (The Brain Tumour Charity, 2018). Headache, often with vomiting, motor abnormalities, and visual changes are typical presenting symptoms of intracranial tumours in older children, but there are many other presentations that may be seen in children, depending partially on age (Wilne et al, 2012). Common symptoms are shown on the ‘Head Smart’ card (Figure 2) and should prompt urgent referral for investigation for a possible brain tumour.
Tumour lysis syndrome
TLS describes a condition of rapid tumour cell breakdown, which is most frequently seen in the context of the initiation of cytotoxic chemotherapy, particularly of haematological malignancies such as leukaemia and lymphoma in which many cells are lysing and releasing their contents (Will and Tholouli, 2011).
TLS is known to occur with other treatments, such as steroid treatment, hormonal therapy, radiotherapy, immunotherapy (for example, monoclonal antibodies) or targeted therapy (Cairo et al, 2010). Spontaneous TLS (that is, before initiation of cancer treatment) has been reported and is mostly associated with high-grade malignancies such as acute leukaemia or high-grade lymphoma (Cairo et al, 2010). In TLS, the lysis of cells causes metabolic derangement, including hyperkalaemia, hyperuricaemia, hyperphosphatemia and hypocalcaemia, which may prove fatal due to the resulting organ dysfunction (Jones et al, 2015).
Patients who are dehydrated and those with pre-existing kidney dysfunction are at higher risk of developing TLS and it is important to closely monitor their renal function.
Superior mediastinal syndrome
Superior mediastinal syndrome (SMS) occurs when the mediastinal contents, notably the trachea and superior vena cava, are compressed by a rapidly expanding tumour, resulting in respiratory and circulatory compromise that may prove rapidly fatal (Seth and Bhat, 2011). The most common cancers causing SMS include non-Hodgkin's lymphoma, ALL and Hodgkin's lymphoma. The condition requires urgent recognition and treatment.
Management
Any child presenting acutely unwell should be assessed and managed using a structured ABCDE approach (Airways, Breathing, Circulation, Disability, Exposure) (Table 2), which is a useful and vital part of the primary survey. Necessary interventions identified at each step should be actioned before assessing the next step (Skellett et al, 2021). This approach includes gathering basic observations of physiological functions and consciousness, which will help to indicate how unstable the patient is. It is important for the health professional assessing the child to request help early, especially if the patient is unstable. If a patient is very unstable and at risk of cardiac or respiratory arrest, a crash call (if the child is in the hospital) should be put out. Once any immediate threat to life has been ruled out or treated, the secondary survey may begin, which involves a focused history and examination. In the paediatric setting, a collateral history is very valuable and it is important to establish the identity and relation to the patient of anyone who is accompanying the child. Specialist management of these conditions are not within the realms of this article and are not included here.
Table 2. ABCDE assessment
| Airways | Patency: voice/breath sounds |
| Breathing | Respiratory rate, oxygen saturations, chest movements, percussion, auscultation |
| Circulation | Skin colour, capillary refill time, pulse rate, blood pressure, ECG, signs of shock |
| Disability | GCS/AVPU, pupil size, blood glucose |
| Exposure | Expose skin – bruising/bleeding/rashes/trauma, temperature |
Key: AVPU=alert, voice, pain, unresponsive; ECG=electrocardiogram GCS=Glasgow Coma Scale
(Source: Skellett et al, 2021)History
Asking relevant questions in the history is important to narrow down the differential diagnoses for a child presenting acutely unwell. Different approaches may be taken, depending on whether the child is known to have cancer or if it is yet to be diagnosed. If the patient is already known to the cancer team, their clinical nurse specialist or paediatric team should be contacted immediately. If the patient is enrolled in a clinical trial, the research nurse and possibly the oncology pharmacist would need to be informed. The family usually will have a file with the names of all the staff involved in the child's care, but they may not have it handy in an emergency situation. The history should include:
- Presenting complaint
- Discuss any obvious issues/changes
- Past medical history
- Does the child have any ongoing medical conditions?
- If they have a diagnosis of cancer:
- Where is the child being managed (that is, if not presenting in the specialist oncology centre)
- What treatment are they taking?
- Have they had any changes or new treatments recently?
- Were they warned about any possible side-effects or complications of treatments, or complications of the condition?
- Questions which may be asked at triage and are likely to provide information on any specific organ system involved include:
- Any change in behaviour/sleep/consciousness?
- Any fits or fainting episodes?
- Any fevers?
- Any cough, difficulty breathing, hoarse voice, noisy breathing?
- Any chest pain?
- Any change in eating or drinking?
- Any nausea, vomiting, diarrhoea or constipation?
- Number of wet nappies/times they visit the toilet?
- Any skin changes: sweaty, cold to touch, rashes, and change of colour?
- Any change in their appearance: swollen face, eye changes?
- Any bleeding?
- Any movement changes: are they able to do everything they can normally do?
Physical examination
When a child presents to the emergency department (ED) in an acutely unwell state, it is always essential to start with the ABCDE approach. Within this approach, the health professional is able to assess and treat any immediately life-threatening signs before a diagnosis has been made. Requesting senior help is vital at this stage. A nurse will typically be one of the first health professionals in a hospital to assess an acutely ill child. Using the ABCDE approach, the triage nurse can assess how unwell a child is and begin to treat certain signs while waiting for senior members of staff to arrive.
The Paediatric Early Warning Score (PEWS) (Agulnik et al, 2017) is a commonly used system to evaluate an acutely ill child. It includes heart rate, respiratory rate, blood pressure, temperature, and oxygen saturations. This information should be collected throughout the ABCDE approach and is a useful baseline for the health professionals to use. The clinician should not move on from the ABCDE approach until all concerning signs have been addressed. A full history and physical examination can then be started by the doctor or a nurse specialist/practitioner to determine the underlying diagnosis/problem.
Investigations
Certain investigations should be considered if an oncological emergency is suspected or expected imminently. This will depend on which emergency is suspected; however, there are some initial investigations that may apply to all acutely unwell children:
- Common blood tests:
- Capillary glucose
- Blood gas
- Full blood count (FBC)
- Urea and electrolytes (U&E)
- Liver function tests (LFTs)
- C-reactive protein (CRP)
- Blood cultures (from a peripheral IV line and a central line if one exists)
- Additional blood tests:
- Lactate dehydrogenase
- Alpha-fetoprotein
- Bone profile
- Uric acid
- Other investigations:
- Urinalysis: in young children presenting with possible infection
- Stool culture
- Fundoscopy: suspected raised ICP
- Electrocardiogram (ECG)
- Imaging:
- Chest X-ray: respiratory symptoms
- CT head: suspected raised ICP
- MRI of head: better resolution image of the brain
- Echocardiogram: cardiac symptoms
- Ultrasound of chest or abdomen: for masses or effusions.
Treatment
The definitive treatment given will be based on the underlying diagnosis, typically made by a specialist. Addressing any problems identified during the ABCDE approach is a priority; this may include administration of oxygen or fluids, or simply gathering information that will be useful in determining the diagnosis. Obtaining peripheral vascular access may be very useful. Raising the head end of the bed to 30° is also an important feature in the management of the child who has suspected or elevated ICP.
Prognosis
The overall 5-year survival rate for childhood cancer is now 82%, with cancer-specific overall survival rates of 100% for retinoblastoma, 91% for lymphoma (Hodgkin's 96% and non-Hodgkin's 88%), 88% for leukaemia (92% for ALL and 69% for AML) and 75% for brain tumours (Children with Cancer UK, 2021). Brain tumours carry the highest mortality of all childhood cancers; this is likely in part due to delayed identification, and the non-specific symptoms such as headache, nausea or vomiting can therefore mimic other less serious childhood illnesses (The Brain Tumour Charity, 2018). The Head Smart campaign has been launched to raise awareness of the signs and symptoms of brain tumours in children in order to reduce time to diagnosis in the UK (Fry et al, 2014).
Supporting families
During an acute emergency, it is important to acknowledge any family members and establish their relationship to the patient. It is preferable to have only a few people around the bedside, and it is helpful if an experienced health professional, preferably a children's nurse, is delegated to stay with the family and keep them, and medical staff, updated about the child's progress. Once the situation has stabilised, it is prudent that the lead clinician and supporting nurse take the time to sit with the family and explain what has happened and what will happen next.
Role of the nursing team
Nurses play an extremely important role in the early recognition and escalation of acute oncological presentations in children, and are greatly involved in parental education, as well as in ongoing management in the community. It is important that nurses use the Children and Young People Oncology/Haematology Triage Tool V2 developed by an expert working group from the UK Oncology Nursing Society (UKONS), the Children and Young People's Cancer Nurses Group of the Royal College of Nursing and the Children's Cancer and Leukaemia Group (UKONS et al, 2020) to remotely provide consistent assessment and advice for parents of a child with cancer. Table 3 provides an overview of the different roles of the nursing team involved in such cases.
Table 3. Role of nurses in managing suspected oncological emergencies
| Nurse | Role |
|---|---|
| School and community nurse |
|
| Practice nurse |
|
| Emergency department nurses |
|
| Children's nurses |
|
| Health visitors |
|
| Paediatric intensive care nurses |
|
Sources: Fry et al, 2014; Brayley et al, 2019
Case studies
Case 1
History
A 10-year-old girl was brought to the GP surgery having felt unwell for 2 to 3 weeks. She had been diagnosed with ALL at age 2½ years and was successfully treated and had been in remission for the past 5 years. Her parents reported noticing bleeding from the gums and easy bruising of thighs, arms and back, despite no history of significant trauma. The girl also reported night sweats and needed to sleep upright in the bed with lots of pillows. The girl was referred to the paediatric team.
Examination
The advanced paediatric nurse practitioner noted that the girl looked pale, and recorded a temperature of 38.1°C, and a respiratory rate of 36 breaths per minute. Her heart rate was 106 beats per minute and she had decreased oxygen saturations of 93% in air. She looked unwell and found it difficult to lie flat for the examination.
What was the immediate priority intervention?
The priority was to stabilise the child using the ABCDE approach, give oxygen and organise blood investigations. The nurse practitioner discussed the child's case with the regional oncology centre to arrange a potential transfer. The patient was encouraged to sit in the position most comfortable for her to breathe.
Differential diagnosis
Possible diagnoses were a recurrence of leukaemia or a new malignancy with superior medistinal syndrome, autoimmune conditions, deep-seated infections (such as osteomyelitis) and tuberculosis.
What are the appropriate investigations in this setting?
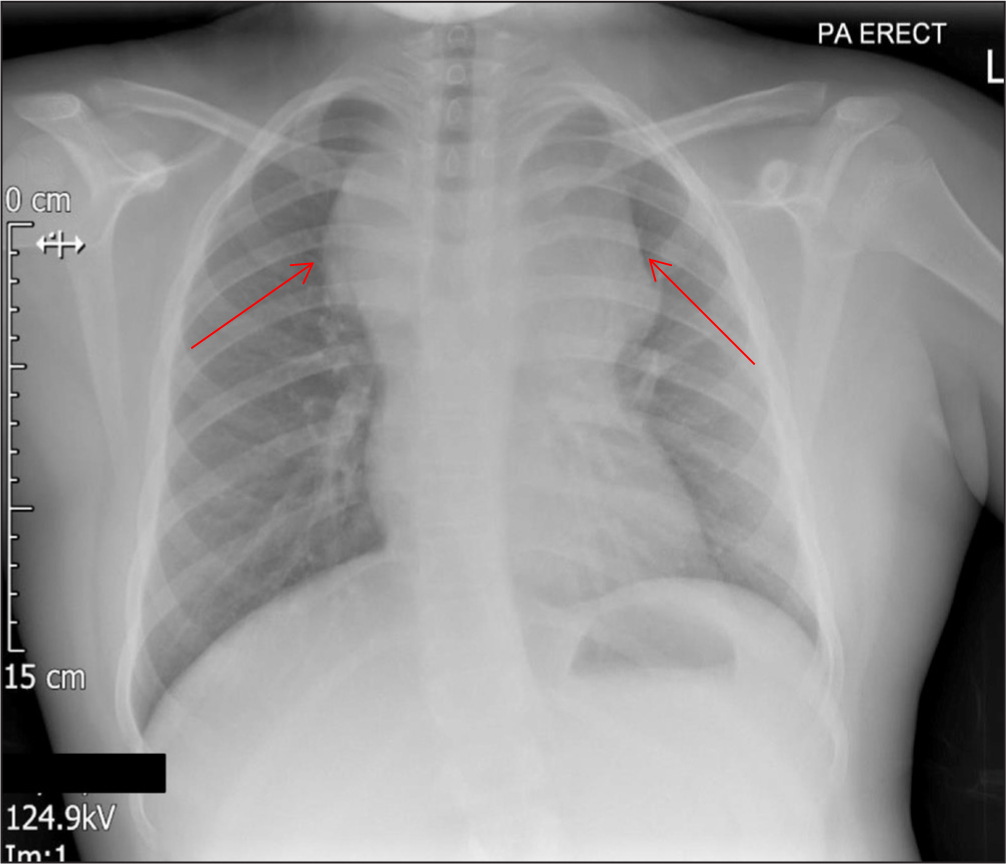
Bloods (FBC, U&E, LFTs, CRP, lactate, uric acid, blood film) were taken and a chest X-ray, which may be normal in such patients. Her chest X-ray showed a large anterior mediastinal mass (Figure 3) known to be associated with leukaemia and is suggestive of superior mediastinal syndrome.
What other steps would need to be considered?
The child was transferred to the regional oncology centre for confirmation of diagnosis and definitive management.
Final outcome
The child's white cell count was 63 x 109/litre and her blood film showed the presence of blast cells highly indicative of a relapse of her leukaemia. Uric acid and potassium were raised at 562 µmol/litre and 6.7 mmol/litre respectively, suggestive of TLS. She was administered allopurinol, intravenous fluids, and transferred immediately to the regional oncology centre, where a bone marrow aspirate confirmed recurrence of leukaemia. She was started on chemotherapy and other supportive management. The child recovered and went into remission.
Case study 2
History
An 8-year-old boy presented to the ED with a 3-day history of headache, 5 days of vomiting, 2 weeks of being unstable on his feet, which had gradually worsened, and 2-3 months of deterioration in his school performance. There was no history of trauma or visual disturbance and the episodes started after a mild viral illness.
Examination
The emergency nurse practitioner undertaking the initial assessment had to support the child, with his mother, to get him on to the examination couch and noted an ataxic gait. Observations were all within normal ranges and he was clinically well hydrated. There was no other focal neurological findings, neck stiffness, meningism or fundoscopic changes.
What was the immediate priority intervention?
The child was stabilised using the ABCDE approach. Particular attention was paid to his blood pressure and pulse rate. The nurse discussed the boy's case with the regional paediatric neurosurgery centre for arranging a potential transfer.
Differential diagnosis
Possible diagnoses included a brain tumour, post-viral cerebellar ataxia and encephalitis/encephalopathy.
What are the appropriate investigations in this setting?
Bloods (FBC, U&E, LFTs, alpha-fetoprotein, lactate dehydrogenase (LDH)) and urgent neuroimaging (CT/MRI scan of the head and brain).
What other steps would need to be considered?
A time-critical transfer to the regional paediatric neurosurgical centre for definitive management. The transfer was done by the local anaesthetic medical team.
Final outcome
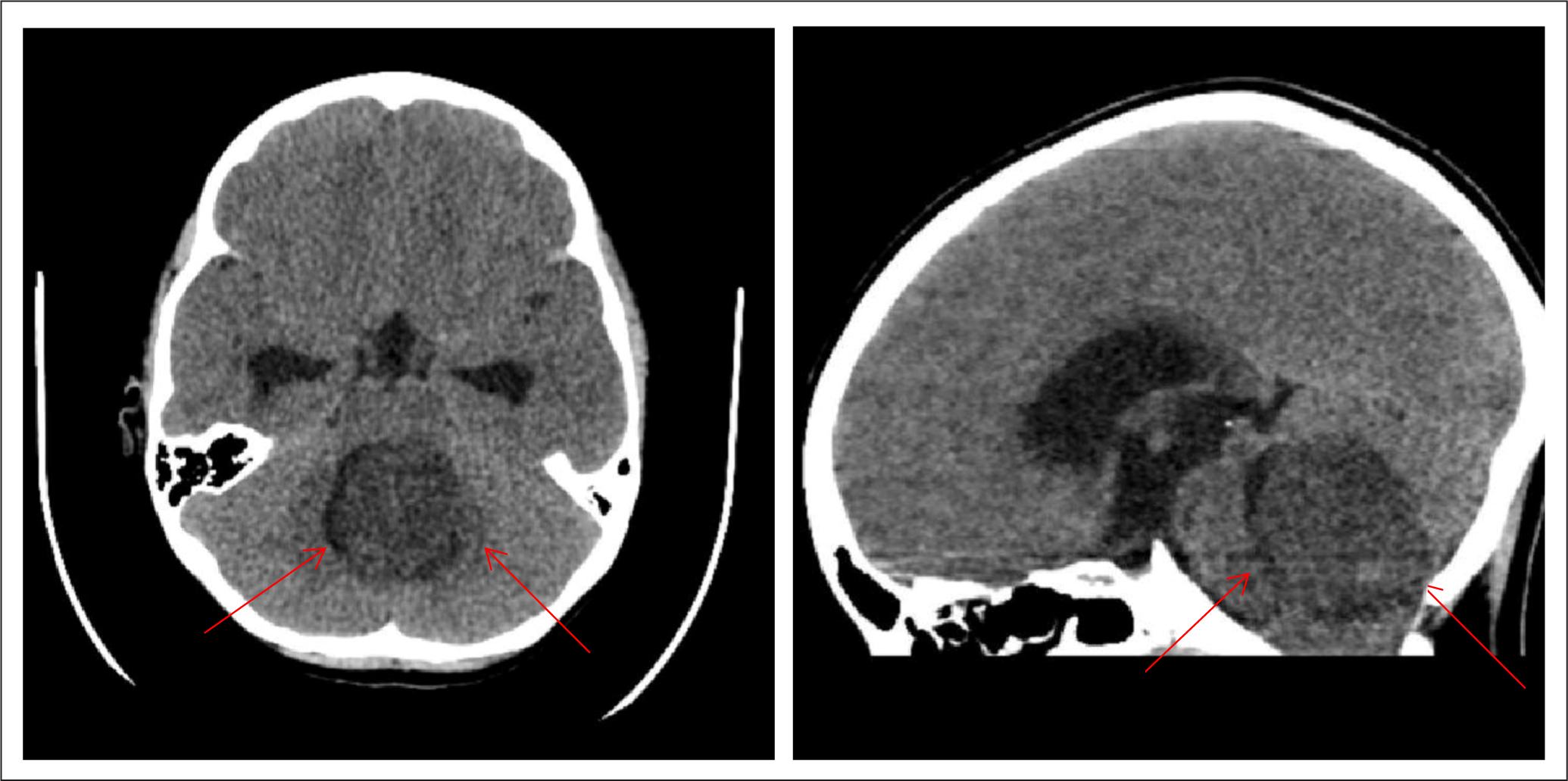
The LDH and AFP blood tests were abnormal. The CT scan of the brain (Figure 4) showed a large mass in the region of the fourth ventricle. There was significant hydrocephalus with dilated ventricles above the mass, subependymal oedema around lateral ventricles and effacement of sulci globally. He was diagnosed with a brain tumour. He was administered intravenous dexamethasone to decrease the swelling and was transferred immediately to the regional neurosurgical centre for decompression surgery and other specialist treatment. He made a good recovery and was discharged from the oncology team 2 years later.
Conclusion
Paediatric oncological emergencies, although rare (except neutropenic sepsis), may present with vague signs and symptoms and benefit from timely recognition and intervention. It is vital to approach an acutely unwell child using the ABCDE approach, and to request help from the appropriate specialist teams at an early stage. NICE guidelines and resources such as Head Smart cards and the Sepsis Symptom Card are helpful adjuncts in recognising and managing oncological emergencies. To be able to manage an oncological emergency well, a multidisciplinary team approach is essential and care should be taken to ensure that the family is well supported and kept updated during such a stressful time.
KEY POINTS
- The ABCDE approach should be used to assess an acutely unwell child
- It is important to contact specialists early when a suspected oncological emergency presents
- Empirical antibiotic treatment should be initiated in suspected neutropenic sepsis without delay or waiting for investigation results
- In a child with suspected raised intracranial pressure, elevate the head end of the bed to 30° and maintain the systemic blood pressure
- Risk stratifying patients can aid treatment decisions
CPD reflective questions
- Think about why it is important to identify oncological emergencies in children early and to be able to differentiate these from other, less serious, self-limiting childhood conditions
- Think about a few challenges you may have faced while managing children with suspected or imminent oncological emergencies and how you have addressed parental worries and expectations in such situations
- Reflecting on the case studies in this article, list a few scenarios where you have identified that nurses working in different clinical settings have made a difference either by recognising the oncological emergencies early or because they picked up deterioration in clinical status post-diagnoses, and therefore escalated concerns to a senior health professional
- The COVID-19 pandemic has presented many clinical challenges: list a few strategies that your centre may have used to manage children with oncological emergencies


