Patient deterioration events are commonly preceded by a period of abnormal vital signs (Lighthall et al, 2009; Fagan et al, 2012; Hands et al, 2013). Among the standard vital signs, growing evidence suggests that respiratory rate (RR) is the most important (Cretikos et al, 2008; Rolfe, 2019). RR is a strong predictor for detection of early patient deterioration (Churpek et al, 2013; 2016), cardiac arrest (Cretikos et al, 2008), and it is an early indicator of hypoxia, hypercapnia, and metabolic and respiratory acidosis (Rolfe, 2019).
Despite its importance in early detection of deterioration, RR is often the least likely vital sign to be monitored or automated, particularly in medical/surgical wards (Leuvan and Mitchell, 2008; Semler et al, 2013; Elliott and Baird, 2019; Palmer et al, 2022). Several studies have reported that RR was missed in the range of 76% to 83% of the times that other vital signs were recorded (McGain et al, 2008; Ludikhuize et al, 2012; Tirkkonen et al, 2013; Cardona-Morrell et al, 2016; Difonzo, 2019). RR is also more likely to be inaccurately recorded, in part because it is not often measured for the full 60 seconds needed for an accurate count (Rimbi et al, 2019; Takayama et al, 2019; Kallioinen et al, 2021).
RR may not be measured and/or recorded due to either a lack of understanding of its importance, a misconception that oxygen saturation is a sufficient substitute, lack of time, or the subjective nature of measuring RR (Hogan, 2006; Philip et al, 2013; Ansell et al, 2014; Mok et al, 2015; Smith and Aitken, 2016; Elliott, 2016; Flenady et al, 2017; Elliott and Baird, 2019). Evidence of the general undervaluing of RR has been found in many studies and from countries spanning Australia to the USA. However, to the best of the authors' knowledge at the time of publication, no studies included representation from multiple countries, making comparisons across countries and regions difficult. Moreover, it remains unclear whether monitoring practices may have been an anomaly in a few institutions and are not representative of country-wide or regional practices.
This article addresses three research objectives and involved an international survey of 161 medical/surgical ward nurses each from a different institution. The three objectives were:
- To measure the perceived prevalence of early detection of deterioration protocols
- To examine which vital sign parameter respondents perceived as the leading indicator of deterioration
- To better understand current practices related to RR monitoring.
Each research objective was examined globally and compared across regions. These findings provide critical insight into current global beliefs and practices related to RR monitoring. Educational initiatives underscoring the value of RR in early detection of patient deterioration could improve nursing practice and, as a result, improve the earlier recognition of patient deterioration and patient outcomes.
Methods
Survey methodology
This descriptive, non-experimental study surveyed nursing professionals (nurse managers, staff nurses) from eight different countries: the UK, France, Germany, Australia, mainland China, Singapore, the Kingdom of Saudi Arabia, and the United Arab Emirates (UAE). Survey responses were completed between 1 December 2019 and 31 January 2020.
The 25-item online survey was developed by DJS Research (Stockport, UK) in partnership with HillRom, Inc (now Baxter International). Questions covered nurse demographics, hospital characteristics, deterioration detection indicators and protocols, and RR monitoring practices within each respondent's facility. All questions were provided in the survey respondent's native language.
This survey was conducted in a double-blinded fashion by DJS Research. No protected health information or personally identifiable information were solicited or collected, and respondents were compensated for their time. Data processing occurred in full compliance with the European Union's General Data Protection Regulations. Participants received an email invitation to participate in the online survey. Participation was voluntary and completing the survey served as informed consent.
Inclusion criteria
The study sample included nurse managers and staff nurses who worked in acute care hospitals with at least 100 medical/surgical beds. Nurses who did not work in direct patient care of adults on medical/surgical wards were excluded. All respondents were required to have prior experience with electric beds and digital vital signs machines. Eligible respondents must have been working in their current role for at least 1 year. Respondents were eligible only if no other respondents had yet participated from their hospital to avoid the potential for oversampling a few hospitals within a country.
Statistical analyses
Responses were analysed by geographic region: Asia-Pacific (Australia, mainland China, Singapore), the Middle East (UAE, Saudi Arabia), and Western Europe (UK, France, Germany). These countries represent a wide variation in healthcare system practices (for example in access to technology, treatment guidelines) and cultures.
Descriptive statistics summarised respondent demographics, including years of respondent experience, hospital funding type, hospital size, country, region, electronic medical record (EMR) use and smartphone use.
To examine the perceived prevalence of early patient deterioration initiatives/protocols, each respondent was asked: ‘Does your medical/surgical setting have initiatives to help with the early detection of patient deterioration?’
To determine whether RR was perceived as a leading indicator for early detection of patient deterioration, respondents were asked to identify which indicators/parameters they used to assess potential patient deterioration. These indicators/parameters included: heart rate (HR), RR, blood pressure (BP), temperature, oxygen saturation (SpO2), an early warning score system (EWS), a visual assessment, telemetry monitoring, end-tidal carbon dioxide rate (EtCO2), or other. These parameters were chosen based on a search of the recent literature on assessing risk of patient deterioration.
First, the five standard vital signs (BP, HR, RR, SpO2, and temperature) were included because these are considered the cornerstone of patient monitoring. Second, EWS systems were included because the combination of multiple physiological changes can determine the severity of illness in a patient. Visual assessment was included as nurses use it in combination with physiological parameters to determine the patient's overall condition, which includes the assessment of skin colour, facial expressions, and other physical and/or mental changes. Telemetry and EtCO2 were included due to their use for monitoring patients with particularly acute respiratory or cardiac conditions, and, in some countries, these technologies are used more routinely to monitor patients in medical units. Finally, respondents were able to document options they felt were missing. The order of these parameters was randomised for respondents, and multiple responses could be chosen. Respondents were then asked to rank the top five in order of importance. Results were summarised as the percentage of respondents who chose each option as the most important indicator.
Finally, to understand current RR monitoring practices, respondents were asked how frequently each of the following parameters were monitored: HR, RR, SpO2, EtCO2, temperature, and BP. Respondents could select from the following options: continuously, every couple of hours, two or three times per day, once a day, less than once a day, or not at all for medical/surgical patients. Responses were allocated in post-processing to either ‘multiple times per day’ or ‘once a day or less’ for ease of interpretation. ‘Multiple times per day’ included continuously, every couple of hours, and two or three times per day, while ‘once a day or less’ included once a day, less than once a day, not at all.
Respondents were asked an open-ended question: ‘In which types of medical/surgical patients do you measure RR?’. Responses were translated and then categorised as either indicating they measured RR for all medical/surgical patients, for one or more specific conditions or as having never measured RR for medical/surgical patients.
Respondents were asked how they measure RR and whether they visually count breaths for less than 60 seconds or 60 seconds or longer.
Results were analysed by country, by region, and globally. Analyses were performed in Stata 17.0 software (StataCorp, 2021).
Results
Survey population
Demographic characteristics of the 161 study respondents are reported in Table 1.
Table 1. Characteristics of survey respondents (N=161)
| Variable | n | % |
|---|---|---|
| Years of experience | ||
| 1−5 years | 38 | 24% |
| 6−10 years | 54 | 34% |
| 11−15 years | 35 | 22% |
| 16−25 years | 24 | 15% |
| Over 25 years | 10 | 6% |
| Hospital funding type | ||
| Not for profit | 6 | 4% |
| Private | 53 | 33% |
| Public/government | 102 | 63% |
| Hospital size | ||
| 100−199 | 32 | 20% |
| 200−299 | 28 | 17% |
| 300−499 | 28 | 17% |
| Over 500 | 71 | 44% |
| Unsure | 2 | 1% |
| Region/country | ||
| Asia Pacific | 57 | 35% |
| Australia | 20 | 12% |
| China | 20 | 12% |
| Singapore | 17 | 11% |
| Middle East | 40 | 25% |
| Saudi Arabia | 20 | 12% |
| UAE | 20 | 12% |
| Western Europe | 64 | 40% |
| France | 19 | 12% |
| Germany | 20 | 12% |
| UK | 25 | 16% |
| Technology use | ||
| EMR | 155 | 96% |
| Smartphone | 115 | 71% |
Key: EMR=electronic medical record
NB: Totals may not add up to 100% due to rounding
Respondents were most likely to have worked in nursing for 6 to 10 years (34%) and work in hospitals with more than 500 beds (44%); most respondents worked in public/government hospitals (63%). The UK had the most respondents (n=25), and Singapore had the fewest (n=17). Most respondents (96%) reported using EMRs in their medical/surgical wards to capture patient information, while 71% reported using smartphones to communicate with caregivers, receive patient status alerts, or receive EMR information.
Early patient deterioration initiatives
Eighty per cent of respondents (n=128/161) indicated that their medical/surgical ward had initiatives to detect patient deterioration early, although results varied by region. For example, every respondent from the Middle East indicated that their facilities had deterioration detection initiatives, while only 67% of respondents in Western Europe indicated this. However, even within Western Europe considerable variation existed, with 92% of UK respondents reporting a deterioration initiative, whereas only 50% of German respondents did so. Table 2 describes results by country and region.
Table 2. Perceived presence of patient deterioration detection initiatives by country/region (N=161)
| Country/region | Respondents reporting initiatives in their facilities (total responses) | % |
|---|---|---|
| Asia Pacific | 45 (57) | 79% |
| Australia | 13 (20) | 65% |
| China | 19 (20) | 95% |
| Singapore | 13 (17) | 76% |
| Middle East | 40 (40) | 100% |
| Saudi Arabia | 20 (20) | 100% |
| UAE | 20 (20) | 100% |
| Western Europe | 43 (64) | 76% |
| France | 10 (19) | 53% |
| Germany | 10 (20) | 50% |
| UK | 23 (25) | 92% |
| Total | 128 (161) | 80% |
NB: Totals may not add up to 100% due to rounding
Most important indicators of patient deterioration
Respondents were asked to select which of nine indicators they used to assess possible patient deterioration. HR was the indicator most frequently selected (n=145; 90%), followed by RR (n=140; 87%), BP (n=138; 86%), SpO2 (n=132; 82%), temperature (n=126; 78%), visual assessments (n=107; 66%), telemetry (n=97; 60%), EtCO2 (n=75; 47%), and EWS (n=69; 43%). Only 21% selected all nine indicators (n=34), while 58% (n=94) reported using at least five standard vital signs (BP, HR, RR, temperature, and SpO2) in their determinations.
Globally (Figure 1), 158 of the 161 respondents then ranked the top five indicators of patient deterioration they used in patient care. Respondents ranked HR highest (n=50/158; 32%), followed by telemetry (n=23/158; 15%), RR (n=19/158; 12%) and BP (n=19/158; 12%). Fewer than 10% of respondents ranked any of the remaining indicators as their top indicator of patient deterioration.
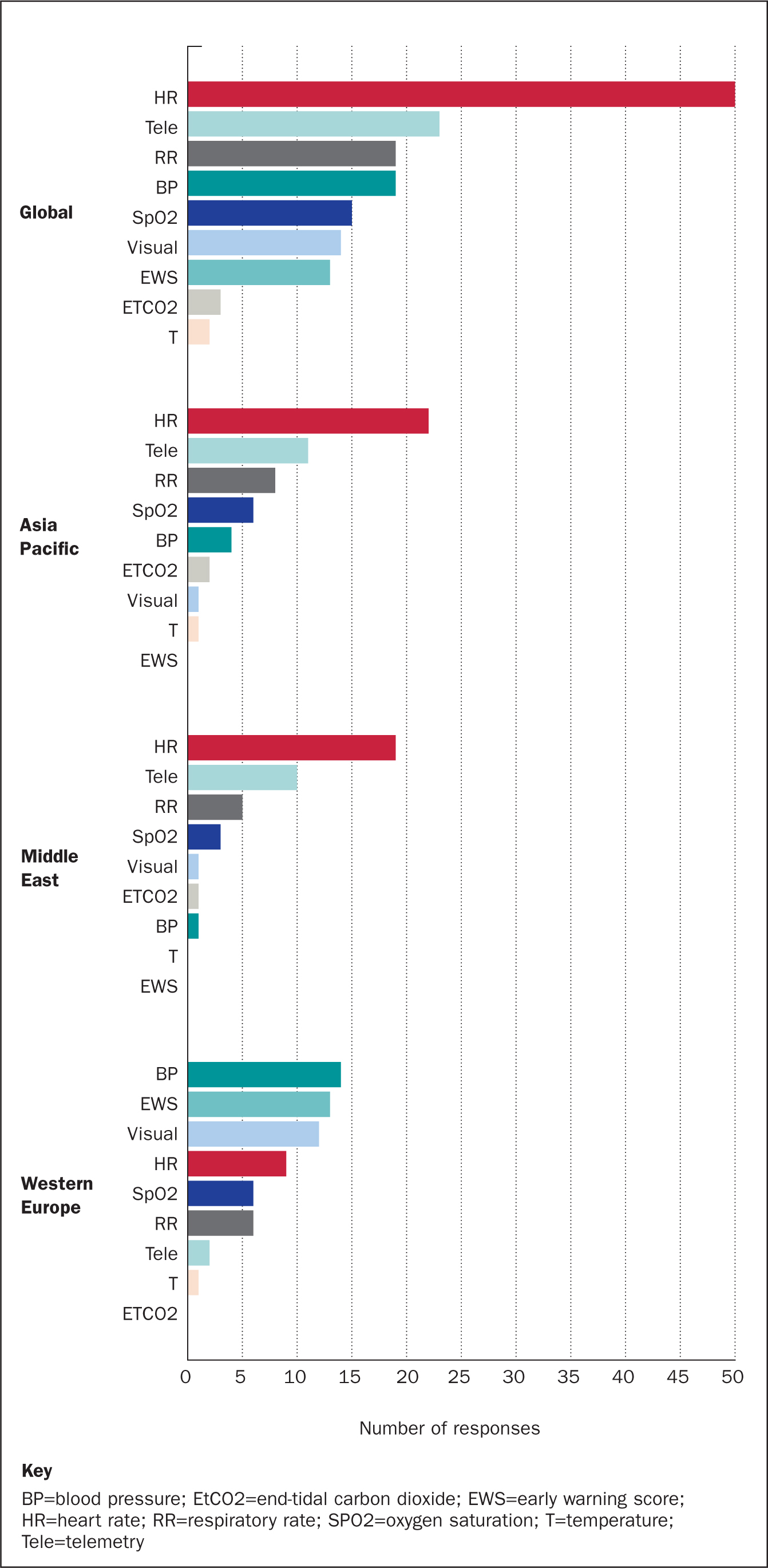
These rankings demonstrated considerable variation across geographic regions. HR was ranked the most important indicator of deterioration by respondents in Asia-Pacific (n=22/55; 40%) and the Middle East (n=19/40; 48%); in these regions, RR was ranked the third most important indicator. In Western Europe (n=63), responses were more evenly distributed across BP (n=14; 22%), EWS (n=13; 21%), and visual assessments (n=12; 19%); nearly 10% (n=6) of respondents ranked RR as their most important indicator of patient deterioration. Figure 1 summarises indicator rankings by region. Full results for countries are available in supplemental materials available from the corresponding author.
Respiratory rate monitoring practices
Nearly all respondents reported measuring patient HR and BP more than once daily (98% and 98%, respectively), while slightly fewer reported measuring temperature and SpO2 more than once per day (94% and 91%, respectively). Of the five standard vital signs, RR was the least likely to be measured more than once per day (n=145/161; 90%). For respondents who reported monitoring EtCO2, only 60% (n=96) indicated monitoring this indicator more than once per day. Full results of 161 are presented in Table 3.
Table 3. Percentage of nurses monitoring vital signs two or more times per day or once or less per day (N=161)
| Vital sign | Two or more per day | Once or less per day |
|---|---|---|
| Blood pressure | 157 (98%) | 4 (2%) |
| EtCO2 | 96 (60%) | 65 (40%) |
| Heart rate | 158 (98%) | 3 (2%) |
| Respiratory rate | 145 (90%) | 16 (10%) |
| SpO2 | 147 (91%) | 14 (9%) |
| Temperature | 151 (94%) | 10 (6%) |
Key: EtCO2=end-tidal carbon dioxide; SpO2=oxygen saturation
NB: Totals may not add up to 100% due to rounding
When asked what types of medical/surgical ward patients they measure RR for, only 27% (n=43/160 responses) indicated they monitored RR for all medical/surgical patients; 68% (n=109/160) indicated they monitored RR for only patients with specific concerns, such as respiratory or cardiac conditions. The final 5% (n=8/160) either never monitored RR or were unaware of when they would need to monitor RR (see Figure 2).
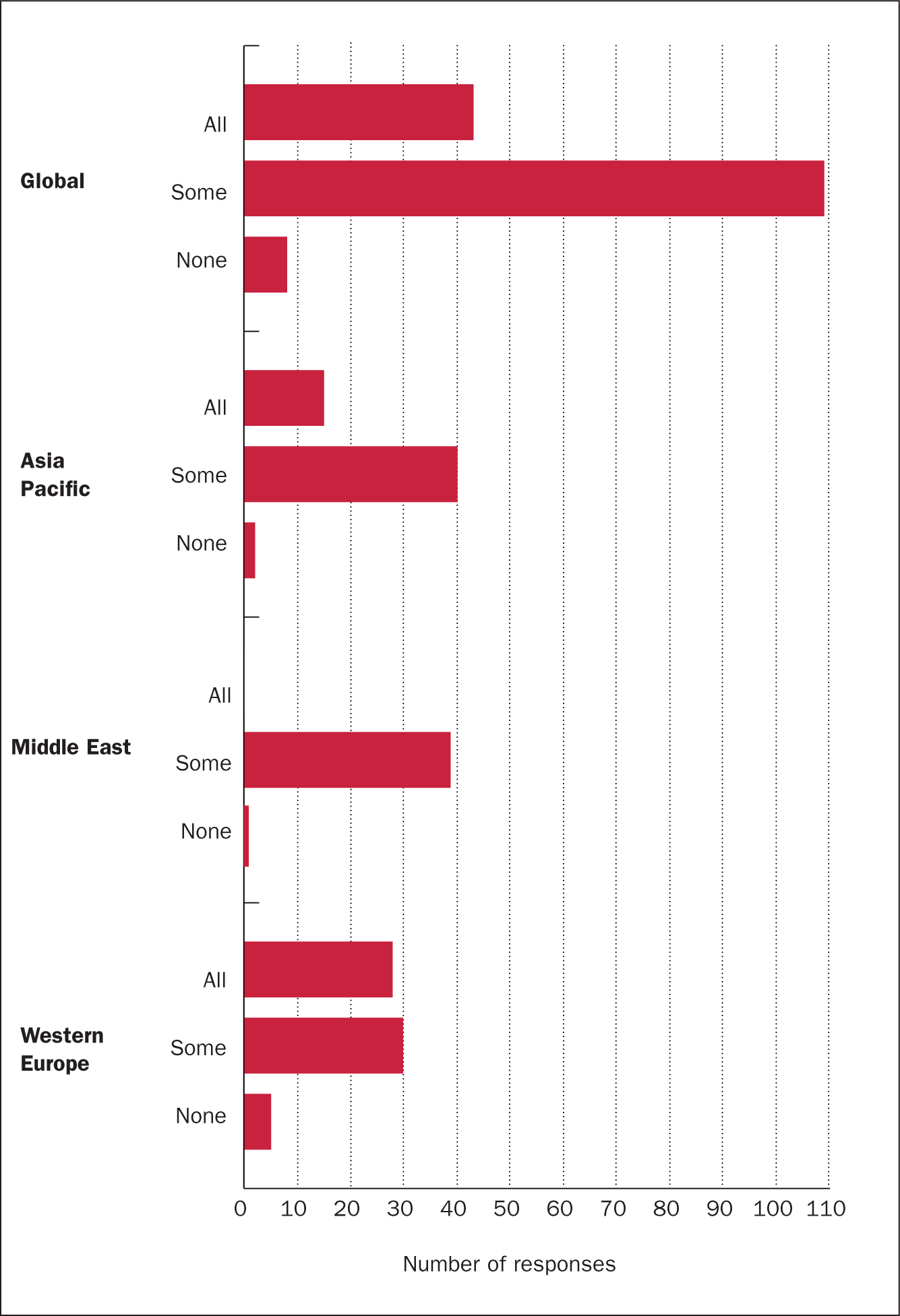
Results varied considerably by country and region. For example, no respondents in the Middle East indicated they monitored RR for all patients compared to 44% of respondents in Western Europe (n=28/63). However, there was considerable variation within the region; 75% (n=18/24) of respondents in the UK indicated they monitored RR for all patients, compared to 25% and 26% of respondents from Germany and France, respectively. Table 4 summarises results by country and region.
Table 4. Respiratory rate monitoring by patient condition and country/region
| Country/region | All patients | % | Condition specific | % | None | % | n |
|---|---|---|---|---|---|---|---|
| Asia Pacific | 15 | 26% | 40 | 70% | 2 | 4% | 57 |
| Australia | 14 | 70% | 5 | 25% | 1 | 5% | 20 |
| China | 0 | 0% | 20 | 100% | 0 | 0% | 20 |
| Singapore | 1 | 6% | 15 | 88% | 1 | 6% | 17 |
| Middle East | 0 | 0% | 39 | 98% | 1 | 3% | 40 |
| Saudi Arabia | 0 | 0% | 19 | 95% | 1 | 5% | 20 |
| UAE | 0 | 0% | 20 | 100% | 0 | 0% | 20 |
| Western Europe | 28 | 44% | 30 | 48% | 5 | 8% | 63 |
| France | 5 | 26% | 13 | 68% | 1 | 5% | 19 |
| Germany | 5 | 25% | 13 | 65% | 2 | 10% | 20 |
| UK | 18 | 75% | 4 | 17% | 2 | 8% | 24 |
| Total | 43 | 27% | 109 | 68% | 8 | 5% | 160 |
Key: UAE=United Arab Emirates
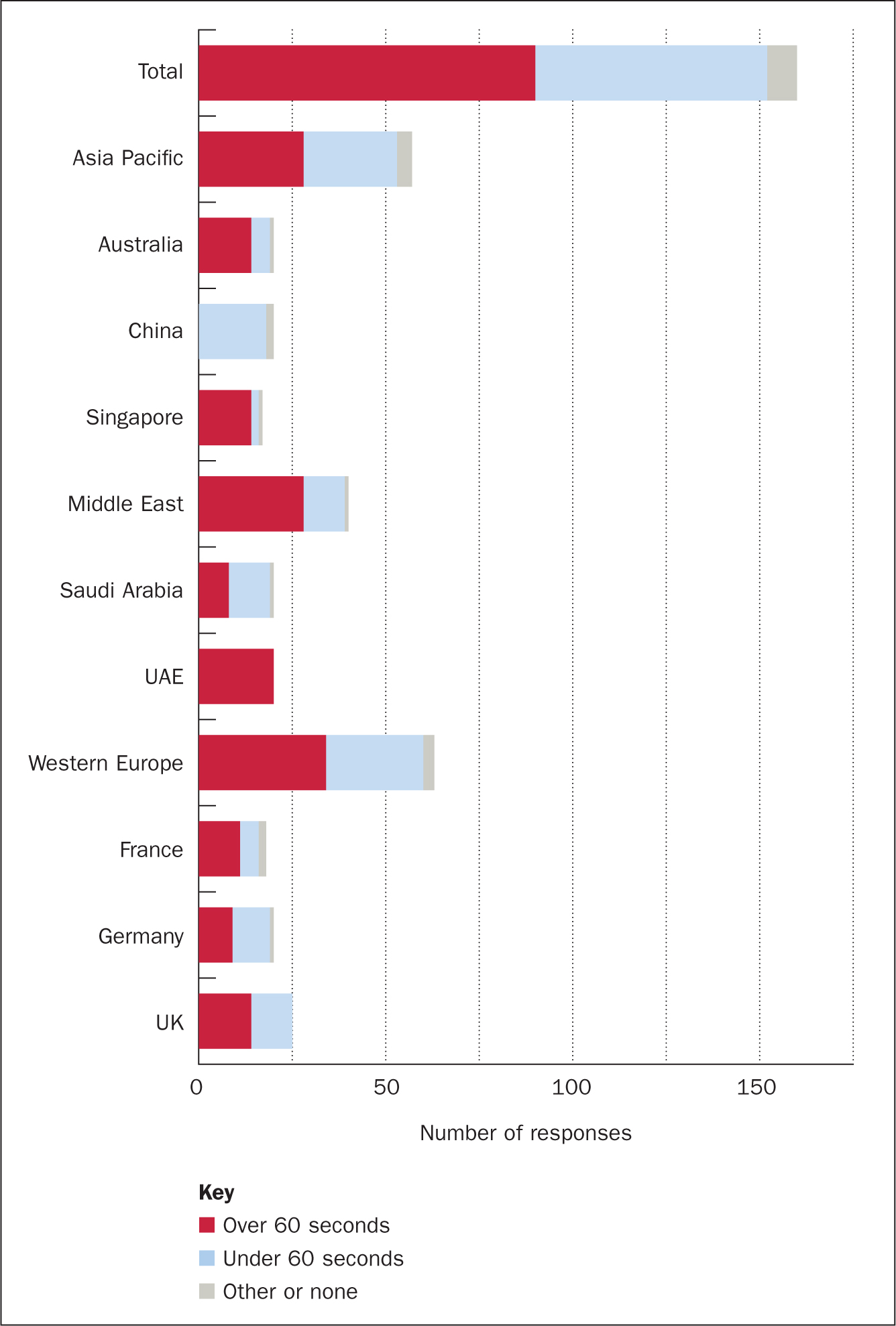
In reporting how they measure RR, just over half (n=90/160; 56%) indicated they monitor RR for 60 seconds or longer compared to 39% who indicated monitoring for less than 60 seconds (n=62/160) and 5% who reported either using a different method or were unsure.
Again, results varied considerably by region and country with 70% of respondents from the Middle East reported measuring RR for 60 seconds or longer (n=28/40). However, within this region, reports varied greatly by country with all respondents from the UAE having reported measuring RR for 60 seconds or longer, compared to 40% of respondents from Saudi Arabia (n=8/20). Similarly, responses varied widely in Asia Pacific with Australia and Singapore reporting 70% and 82% measured RR 60 seconds or longer respectively, yet 0 respondents in China reported measuring RR for 60 seconds or longer. Responses varied considerably less within Western Europe, where 45%, 56%, and 61% of respondents reported measuring RR 60 seconds or longer in Germany, UK, and France respectively. See Figure 3 for results of RR monitoring technique by country and region. All counts and percentages are available in supplemental materials.
Discussion
This study investigated patient deterioration detection initiatives and vital sign assessment practices in medical/surgical environments in Asia-Pacific (Australia, mainland China, Singapore), the Middle East (UAE, Saudi Arabia), and Western Europe (France, Germany, UK). Survey respondents represented 161 unique medical/surgical wards in hospitals with at least 100-bed capacity and where both EMR and smartphones were commonly used.
Perceived prevalence of early patient deterioration initiatives
Most respondents (80%) reported that their medical/surgical ward had implemented initiatives for early detection of patient deterioration including EWS tracking such as the Modified EWS (MEWS) or the National EWS (NEWS2). Although most respondents indicated having at least one such initiative in place within their unit, vital signs' monitoring practices and methodologies varied greatly by region and country.
Most important indicator of patient deterioration
Abnormal RR is a sign of both hypoxia and metabolic acidosis and therefore indicates failure of a multitude of systems (Cretikos et al, 2008). High rates can be the first sign of sepsis and shock and low rates can indicate opioid overdoses (Kellett and Sebat, 2017). RR is a strong predictor of in-hospital cardiac arrest (Fieselmann et al, 1993; Cuthbertson et al, 2007; Cretikos et al, 2008; Churpek et al, 2012), early deterioration (Churpek et al, 2013; 2016), intensive care unit transfer (Kipnis et al, 2016), and is the best physiological parameter to differentiate between stable and at-risk patients (Subbe et al, 2003).
Despite this evidence, this study found nurses were most likely to identify HR as the most important indicator of patient deterioration (n=50/158; 32%). And whereas most respondents said they used RR as an indicator of patient deterioration (n=140/161; 87%), only 12% viewed RR as the most important indicator. These results are consistent with other studies that have found RR is systematically undervalued by nurses (Mok et al, 2015; Elliott and Baird, 2019).
Respiratory rate monitoring practices
Of the five standard vital signs, the present survey found RR was the least likely to be monitored more than once per day (n=145/161; 90%). Nearly all respondents (98%) stated HR and BP were monitored more than once per day, while 94% reported that temperature was monitored more than once per day. In a systematic literature review, Difonzo (2019) found that RR was consistently the least likely of the vital signs to be documented, with a recording rate typically between 14% and 17%. These findings highlight the possibility that these survey results found a higher prevalence of RR documentation than what is happening in practice given the survey asked nurses how often they capture each indicator of deterioration.
Although 87% of study respondents reported that RR is an important indicator of deterioration and 90% said they capture RR two or more times per day, only 27% of respondents (n=43/161) indicated RR was captured for all medical/surgical ward patients. Most respondents (63%) indicated that they captured RR only for patients with specific conditions and not for every medical/surgical ward patient despite recording a full set of vital signs (HR, BP, RR, and temperature) at least daily is considered standard care for all acute care patients (Cretikos et al, 2008). Finally, the survey found only 56% (n=90/160) of respondents reported taking 60 seconds or longer to measure RR, which is recommended for an accurate reading and for identifying deteriorating patients (Rimbi et al, 2019; Takayama et al, 2019; Kallioinen et al, 2021).
Limitations and future research
This study had several limitations. First, although the survey was translated into the respondents' native languages, it was not possible to eliminate all variability in how respondents interpreted the questions. Second, the study was subject to possible selection bias as nurses who responded might be more knowledgeable regarding patient deterioration than those who did not respond. Third, self-reported measurements of vital sign monitoring practices could have been impacted by recall errors or common method bias. Respondents may have felt compelled to report their belief that all indicators of deterioration are important or to overestimate the rate at which they capture these indicators, possibly inflating some of the results. Fourth, limiting the sample to one respondent per hospital prevented overlap in responses, but did limit the sample size and may have impacted the generalisability of the results. Finally, the relatively small sample sizes within each country and region make it difficult to generalise results and limits the authors' ability to interpret differences between countries and regions.
It is important to note that there are other parameters that help nurses identify patients at risk of deterioration. In fact, six respondents documented urine output and blood results. Early warning scores such as the NEWS2 includes whether the patient's level of consciousness has changed (Smith et al, 2019). MEWS includes patient's urine output and level of consciousness (Morgan et al, 1997). Future research would benefit from examining nurse monitoring practices related to these parameters. Finally, different education systems across countries and different healthcare system structures may lead nurses to over or under emphasise RR. Educators could leverage insights from future work comparing different nursing education systems and their vital sign monitoring practices.
Conclusion
This study reinforces the importance of enhancing international nursing education regarding the significance of RR as the most important leading indicator of patient deterioration. Most nurses who responded to this survey reported that their ward had an initiative for the early detection of patient deterioration. However, the results suggest that many nurses may view HR as the most important indicator of deterioration. Not only was HR the vital sign most likely to be listed as the number one indicator of patient deterioration, but it was also the vital sign most likely to be taken more than once per day. Although 90% of responding nurses said they capture RR more than once per day, only 27% reported capturing RR for all patients, and only 56% reported taking the full 60 seconds to capture this vital sign. To improve early detection of patient deterioration, nursing education should be enhanced to emphasise the importance of capturing RR often and accurately for all patients.
KEY POINTS
- Most hospitals have protocols to help nurses detect early signs of patient deterioration
- Those protocols typically involve the monitoring of standard vital signs for all patients
- Growing evidence suggests respiratory rate (RR) is the strongest of the standard vital signs for predicting early patient deterioration
- However, RR is often undervalued by nurses, leading to it often being missed or inaccurately recorded
- Furthermore, RR monitoring practices vary considerably across regions and international guidelines are needed to promote improved recording of RR
CPD reflective questions
- How do the practices in your own clinical setting relate to those described in the study?
- Do caregivers in your clinical setting view respiratory rate (RR) as a leading indicator of patient deterioration?
- What barriers prevent your clinicians from monitoring RR accurately for all patients?

