In many developed nations, healthcare systems are increasingly burdened by rising patient numbers, an ageing population, and technological advances in medicine. The demand for acute hospital beds often exceeds capacity, forcing healthcare providers to explore alternative models of care that offer comparable clinical outcomes while alleviating pressure on hospitals. The ‘Hospital in the Home’ (HITH) model has emerged as an innovative solution to address these challenges, delivering hospital-level care in the patient's home and substituting for inpatient admission.
The popularity of HITH is reflected globally, particularly in the UK, where initiatives such as ‘Hospital at Home’ have achieved measurable success. For example, a service in southwest London, launched in 2021, saved an estimated 2134 hospital bed days in its first year (Central London Community Healthcare NHS Trust, 2022). HITH offers an acute clinical service that delivers hospital-level care outside of traditional inpatient settings. However, it is crucial to distinguish HITH from ‘virtual wards’, which focus on remote monitoring of chronic conditions. HITH, by contrast, emphasises short-term, acute care at home (UK Hospital at Home Society, 2025). Although in the UK this excludes outpatient parenteral antimicrobial therapy (OPAT), which is typically managed by its own team (often staffed by infectious diseases specialists), in Australia the definition does in fact encompass OPAT due to variations in healthcare service provision.
This article provides a detailed account of the evolution of the HITH service in the South Western Sydney Local Health District (SWSLHD), which has been operational since 1998. Set against the backdrop of a socioeconomically disadvantaged region, the service has been instrumental in reducing demand for hospital beds while providing timely, patient-centred care. Through this analysis, the authors explore the contextual factors that have shaped the service's development and offer insights into its broader implications for healthcare delivery in Australia.
The Australian healthcare landscape
The Australian healthcare system is characterised by a combination of public and private services, funded through federal and state contributions, private insurance, and out-of-pocket payments by patients. Unlike the UK's NHS, which provides universally free care at the point of use, Australia's mixed model means that access to some healthcare services, particularly specialist care, often involves significant personal expenses. Public hospitals are primarily funded by the government, but access to specialist services, which are frequently privately run, may require patients to cover out-of-pocket costs even with Medicare rebates.
This financial burden is particularly pronounced in low-income areas such as South Western Sydney, where reliance on public hospitals is high, further increasing pressure on inpatient services. Against this backdrop, the HITH service plays a critical role in alleviating demand for hospital beds by managing patients at home when they are medically stable but still require ongoing treatment.
Development of the HITH service in South Western Sydney
Liverpool Hospital, a tertiary referral centre in South Western Sydney, serves a population of over 1 million people, many of whom face significant socioeconomic challenges. The 2021 Australian Census reported that the local government area of Liverpool had higher-than-average unemployment rates and lower income levels compared with state and national averages (Australian Bureau of Statistics, 2025). This socioeconomic deprivation places increased demands on public healthcare services, making the HITH model particularly relevant.
The HITH service at Liverpool Hospital was initially established to provide OPAT for patients who were medically stable but required long-term antibiotic therapy. Over time, the service has expanded its scope to include a variety of clinical conditions, such as intravenous (IV) immunosuppressive therapy for patients with autoimmune disorders, IV fluids for patients with hyperemesis gravidarum, and advanced wound care, including vacuum-assisted closure dressings. The integration of these services into HITH has reduced the need for inpatient care, freeing hospital beds for patients with more complex or unstable conditions. The cost-benefit analysis of managing diabetic foot disease through OPAT, as described by Malone et al (2015), highlights the economic and clinical efficacy of HITH programmes.
Structure and function of the service
The HITH model is designed to provide hospital-equivalent care to adult patients that meets National Safety and Quality Health Service (NSQHS) Standards (Australian Commission on Safety and Quality in Healthcare, 2021) in the home setting, offering a safe and effective alternative to inpatient care for patients who meet specific clinical criteria.
Inclusion criteria for HITH – current at time of writing – include (NSW Health, 2017):
Patients can enter the HITH service directly from the emergency department (ED), via inpatient transfer, or through referrals from GPs. Working closely with GPs ensures early intervention and facilitates hospital avoidance, particularly for patients who can begin treatment at home without the need for hospital admission. GPs have access to the HITH service via phone, fax or email referrals, allowing for seamless communication between community healthcare providers and the hospital. This collaboration enables HITH to play a dual role: preventing unnecessary hospital admissions and facilitating early discharge from inpatient wards.
Although the service does not specifically exclude children from its patient cohort, at present no paediatricians are a part of the HITH team and cases are evaluated on an individual basis. For example, if the HITH requirement is simple wound management, which can be evaluated and monitored safely by an appropriately trained nurse, then it may be considered as a suitable HITH case.
Exclusion criteria include:
Patients deemed ineligible for HITH care are managed through conventional inpatient pathways, ensuring that those who require closer monitoring or more intensive interventions receive the necessary care within the hospital setting.
The services provided by HITH range from IV medications, injections, anticoagulation management, and wound care to post-acute care interventions. These services are delivered by a multidisciplinary team, including doctors, nurses and allied health professionals, ensuring that all aspects of patient care are covered.
The governance of the HITH service at Liverpool Hospital is robust, with daily nursing reviews and weekly medical assessments to monitor patient progress. Patients are reviewed by HITH staff in person or via telehealth technology, depending on their condition. This comprehensive approach to patient monitoring ensures that any clinical deterioration is identified early, allowing for rapid escalation of care when necessary.
Challenges and limitations
Although the HITH model has proven to be a valuable component of healthcare delivery, it is not without its limitations. One of the primary challenges faced by the Liverpool HITH service is the discrepancy between the number of allocated virtual beds (20) and the actual number of patients managed at any given time (approximately 50). This creates a strain on resources and requires careful co-ordination between HITH staff and community nurses. Additionally, the reliance on daily in-person reviews for all patients can place significant demands on staffing, particularly in regions with high patient volumes.
Another challenge is the need for stringent patient selection criteria. Although HITH provides a safe alternative to hospital admission for many patients, it is essential that only those who meet the clinical criteria are admitted. Patients who are medically unstable, require complex care beyond the capacity of HITH, or have unclear diagnoses may not be suitable for the service. Ensuring that HITH is used appropriately for the right patients is critical to maintaining the safety and efficacy of the model.
Clinical responsibility and remote monitoring
The issue of clinical responsibility is particularly important in the HITH model. Although the service allows GPs to refer patients directly, the clinical oversight remains with the hospital-based HITH team. This ensures that patients receive consistent care and that any deterioration is managed promptly. The introduction of remote monitoring technologies could further enhance the capacity of HITH to manage higher patient volumes while maintaining safety standards. Telehealth consultations, wearable devices, and remote monitoring of vital signs are areas that could be explored to expand the scope of HITH and reduce the burden on hospital services.
The Liverpool experience: outcomes and future directions
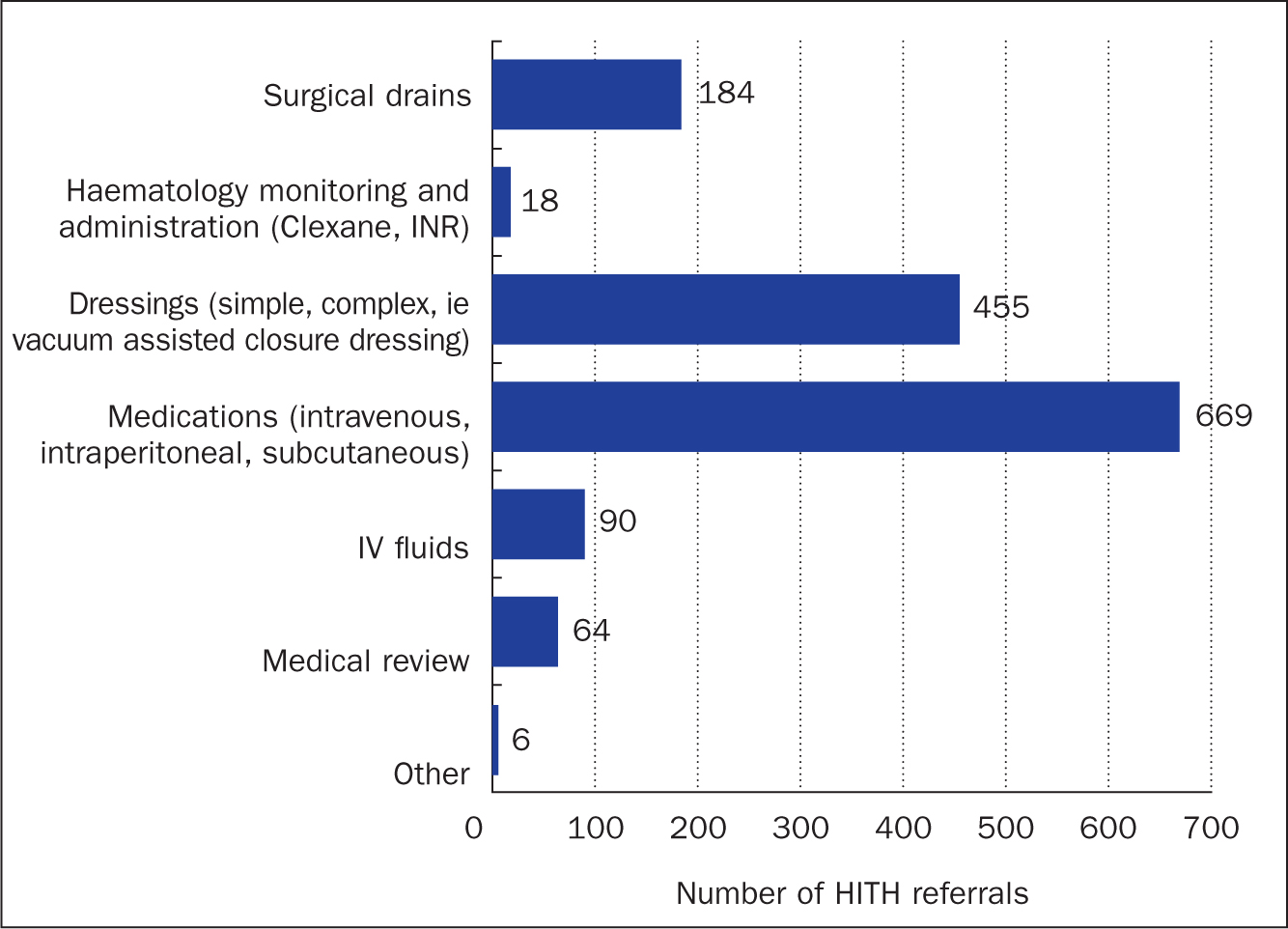
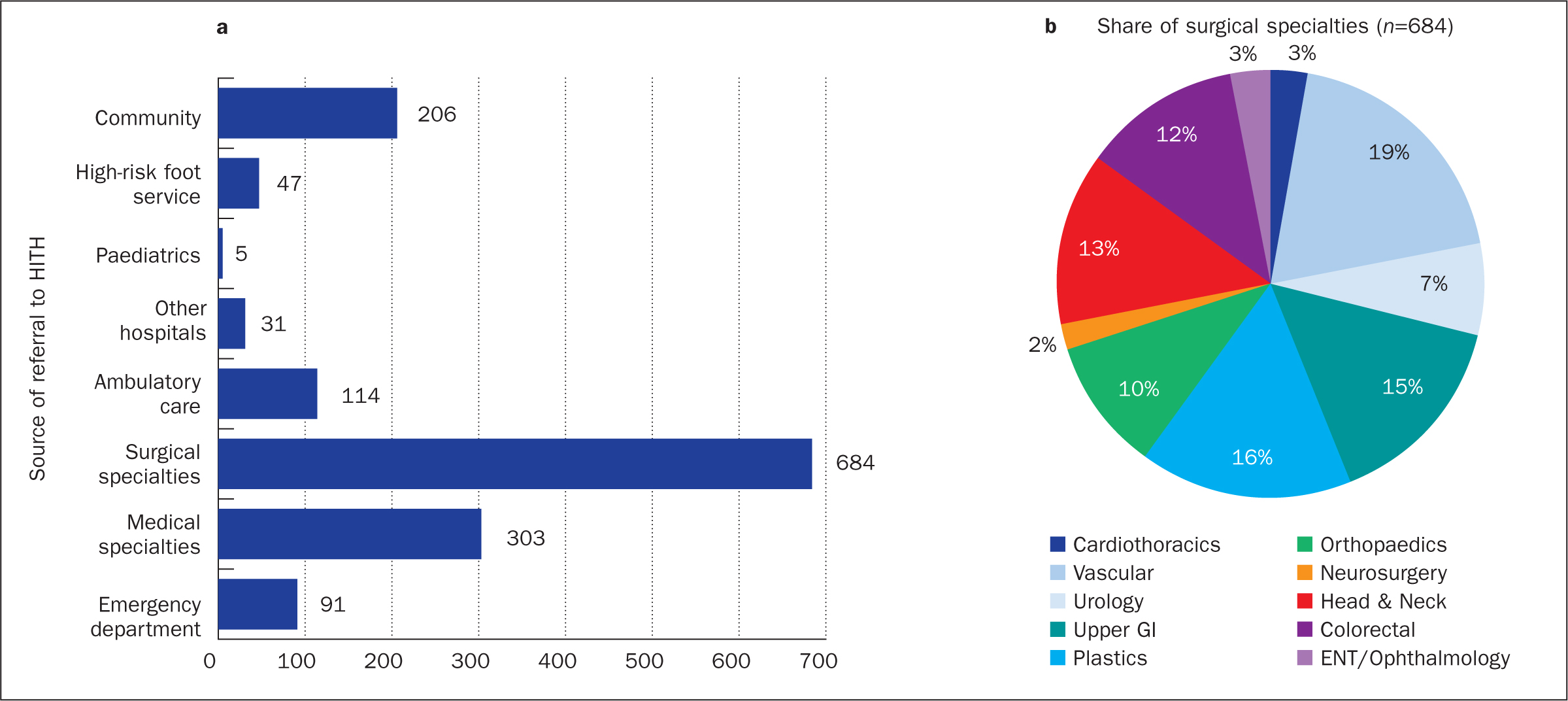
Since the formal establishment of the HITH programme at Liverpool Hospital in 2016, the service has grown steadily in both scope and capacity. In 2020, 1752 patients were admitted to the service, a significant increase from 1132 in 2017 (Figure 1). The top referral conditions in 2022 included IV antibiotic administration, IV bolus antibiotics via elastomeric pumps, and wound management. Figure 2 shows the scope of services delivered for 2023. Figure 3 shows a breakdown by referrer. The service's ability to manage these conditions at home has significantly reduced the demand for hospital admissions, improving bed availability for patients requiring more complex care.
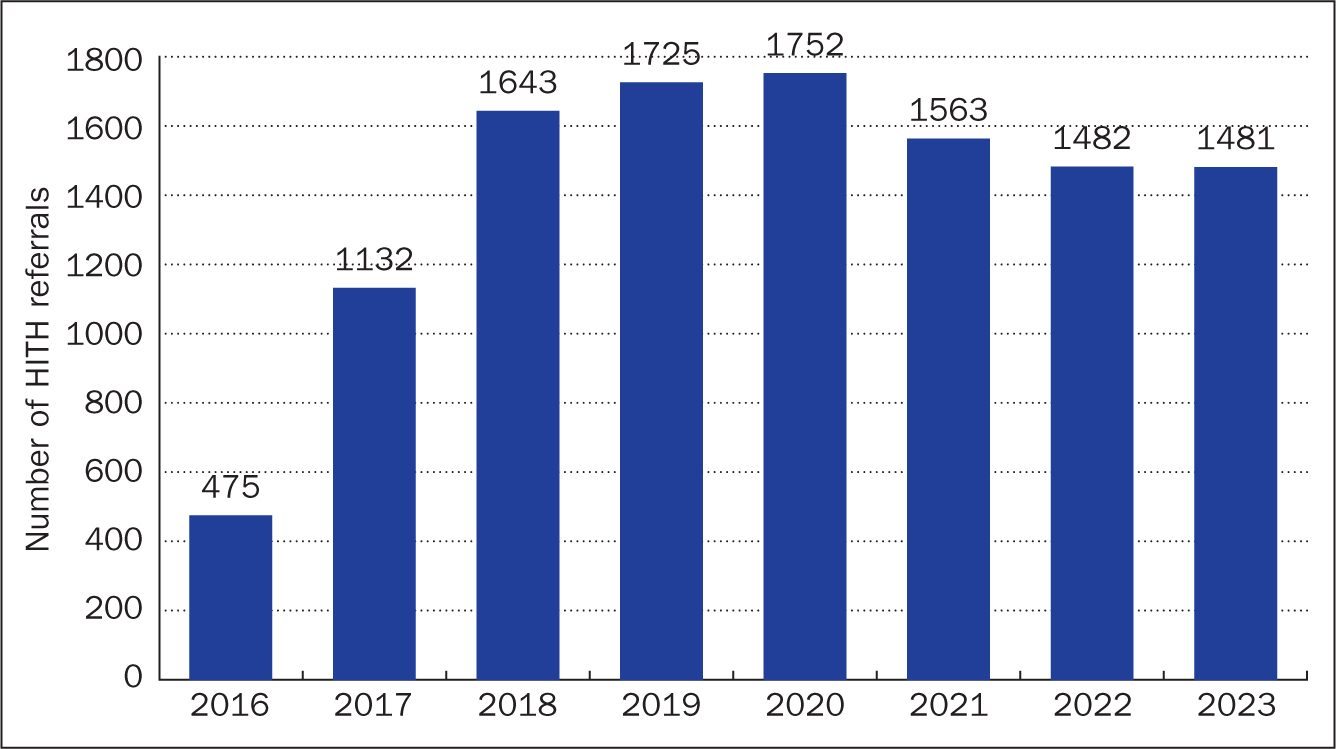
However, the COVID-19 pandemic posed challenges for the service, with patient numbers declining to 1482 in 2022 due to the increased difficulty in delivering acute care at home. Despite these challenges, the HITH model remains a critical component of healthcare delivery in South Western Sydney, with future recommendations including the expansion of remote monitoring capabilities and the integration of more specialised care into the service.
Since this article was written, the NSW Health Admission Policy 2017 has been rescinded and replaced as of March 2025 by the Patient Admission and Discharge to NSW Health Facilities Policy Directive Patient Admission and Discharge to NSW Health Facilities (NSW Health, 2025). This now includes a direct reference to HITH and is supported by a new Hospital in the Home Policy Directive, available at Hospital in the Home effective from 18 February 2025, which advocates for a centralised access point to HITH services in those hospitals that run a HITH service. In terms of how it affects the HITH service at SWSLHD, pragmatically nothing will change in how the team runs the current service, although we are looking to increase our staffing capacity.
Conclusion
The HITH service at South Western Sydney Local Health District exemplifies the potential of innovative healthcare models to address the growing demand for hospital care. By providing acute-level care in patients' homes, HITH has demonstrated its value in reducing hospital admissions.

