Medication errors are a potential cause of harm to hospitalised patients. Medication error is an umbrella term that covers mistakes occurring at different stages of the complex process of prescribing, dispensing, preparation and administration. Many hospitals have policies mandating a double-check at specified stages of administration, with a view to improving safety by building in an opportunity for errors to be identified and rectified. These assume that there are no problems with having the resources to do so, including personnel or time constraints.
The process of double-checking involves two individuals independently assessing information and performing a set of actions in response to that information. This information may be in the form of written material (eg prescriptions and approved administration instructions) and be found on products themselves and include patient identity, as well as parameters such as allergy status on the patient's record. If double-checking is to be effective, it relies on two assumptions:
- Two individuals verify the information independently
- Involving two individuals increases the chance of detecting and rectifying an error, where an error exists.
Policy relating to double-checking is not standardised across the NHS. Many organisations mandate this before the administration of intravenous or subcutaneous medicines, controlled drugs or clinical trial medications as well as high-risk pharmaceuticals, which are those with the most potential for causing harm to the patient in the event of an error.
Many nurses believe double-checking is an effective way to minimise drug errors (Schwappach et al, 2018). Despite this being a difficult area to study rigorously and empirically, work by Kruse et al (1992) and Subramanyam et al (2016) indicated that second-checking may be effective in preventing errors. As medication checking is a human process, there will be an inherent error rate associated with both the first and the second checks, even if these processes are carried out truly independently.
However, a systematic review by Koyama et al (2020) concluded there was insufficient evidence to show that double-checking of medication was associated with a lower number of medication-related errors reaching the patient. Westbrook et al (2010) and Hayes et al (2015) reported a medication administration error rate of 20–25% of doses administered, although only a fraction of these will be detected by error reporting systems and be associated with harm to the patient. Most errors occur because of a combination of factors, which include (Tang et al, 2007):
- Staff having multiple, competing priorities
- Using system one thinking (fast, automatic and intuitive approach with limited voluntary input that does not involve an analytic process) in the context of undertaking familiar and routine tasks
- Experiencing interruptions and distractions
- Lacking knowledge about medication.
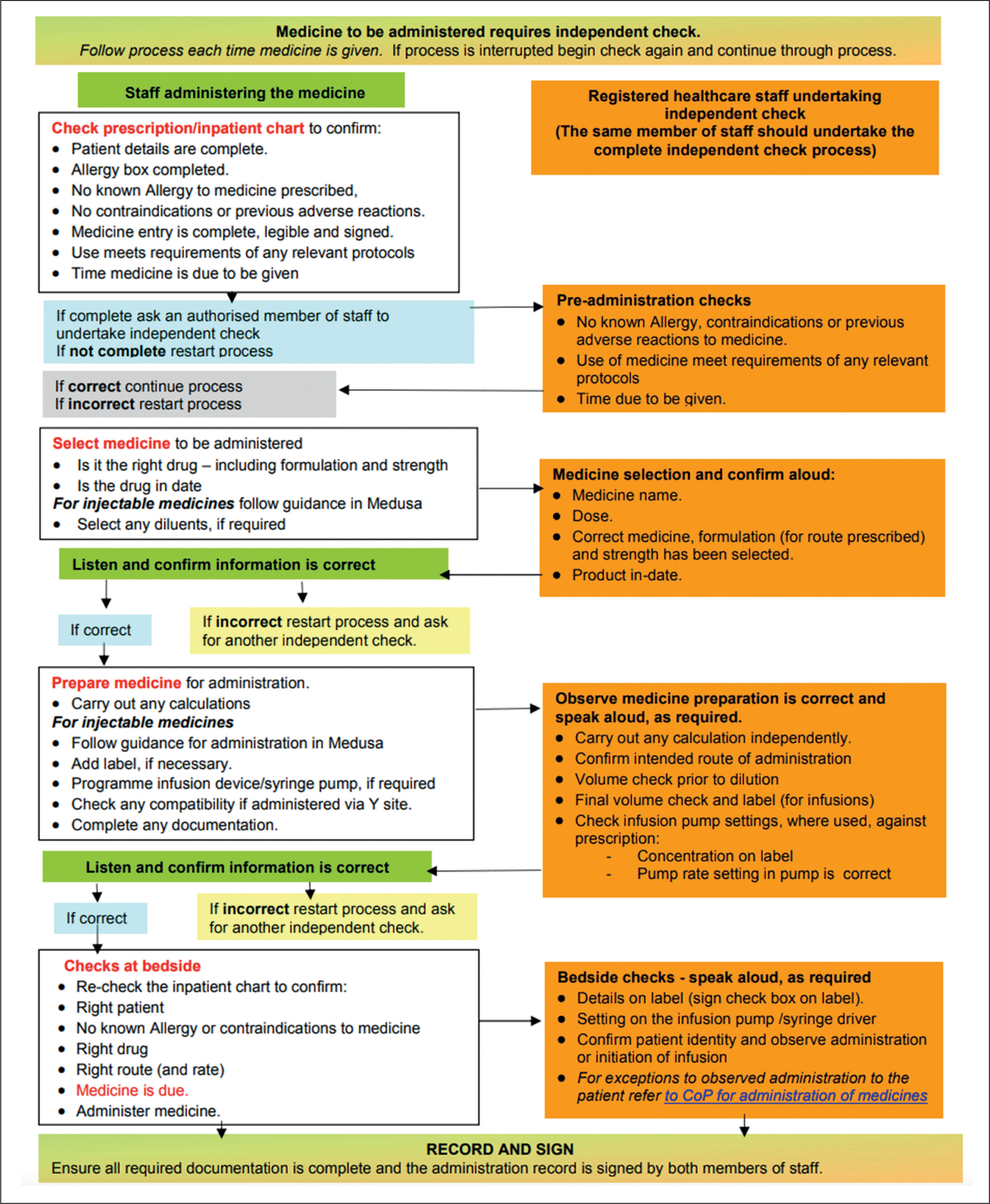
Double-checking is associated with costs, particularly in terms of nursing time and the potential for diverting time to undertake it, and hence away from other clinical activities. Organisational medicines policies are often, by necessity, prescriptive. The process of medication administration is complex, and the relevant policies may be difficult to adhere to consistently, given local realities and matters arising in the course of caring for a critically ill patient on a busy unit. An example of a medication checking process is shown in Figure 1.
As technology advances, the role of a two-person double-check may diminish as technological solutions, such as barcoded medication administration, may in some circumstances take the place of one of the human checkers.
Some organisations already permit the administration of medication following only a single-person check. If single-person checks were implemented more widely, it would be important to account for factors that may facilitate or prevent them from being effective in identifying errors before they reach the patient; any risks must be balanced against benefits to releasing nursing time.
The work described in this article arose out of a local need to update the understanding of a long-standing item on the authors' Trust's risk register: ‘checking and administration of all drugs in critical care’. The vast majority of medication administrations occur without incident and this work was undertaken principally to learn from the experiences of those involved in the breadth of medication administration events. The aim of this work was to identify what critical care nurses feel are the matters that facilitate or prevent them from performing a robust, independent second check when administering medication to critically ill patients, as described within the local medicines policy, across the breadth of their practice.
Method
An exploratory design was adopted for this work, using a focus group method to generate data and an interpretative approach to analysis to gain an understanding of the reality experienced by nurses of the barriers and facilitators to undertaking a robust, independent checking process when administering medication in the intensive care unit (ICU).
Over a span of 6 weeks, four focus groups were conducted by two pharmacists from the critical care pharmacy team. These pharmacists are responsible for clinical governance tasks including the investigation of administration incidents, as well as the dissemination and implementation of solutions. Practising critical care nurses attending their twice-per-year general update day were invited to participate in voluntary focus groups. All were on band 5 or 6 and were working in a variety of ICU and high-dependency units at one organisation.
The purpose, structure, content and recording of the focus group were explained to the potential participants, then everyone was given the option to stay and take part in the group or leave the room while it took place. Focus group conversations were recorded using an electronic recording device. One pharmacist was tasked with leading the discussion while the other took notes and was responsible for operating the technology to record the conversations.
The participants were asked to discuss in a group conversation style, with a pharmacist providing prompts to build the conversation using a topic guide. The topic guide (Table 1) was used as a framework but not adhered to rigidly in order to allow the conversation to flow and draw out and develop points of interest to the group, and to give space for individuals to voice their own anecdotes and describe their experiences. The four sessions were run on the same day as departmental updates and each nurse participated only once. On completion of each session, the audiorecorded notes were transcribed by a pharmacist, with each session on a separate Word document; the pharmacists then met to discuss the key points.
Table 1. Questions in the topic guide the facilitating pharmacist could ask during focus groups
| How questions were phrased | |
|---|---|
| 1 | Among yourselves, discuss what you do when you are checking an intravenous drug as the first checker |
| 2 | What are the barriers to doing the first check according to the medicines policy? |
| 3 | When doing the second check, do you do anything differently? |
| 4 | What are the differences between checks during the day shift versus the night shift? |
| 5 | Is the checking process any different if a senior person is checking? |
| 6 | Is the checking process any different if you are familiar with the drug? |
| 7 | Is the checking process any different if the patient has a high acuity? |
| 8 | Does the location of the patient affect the checking process? |
| 9 | Is the checking process different if the drug monograph is available on Medusa*? |
| 10 | Do you think the medicines policy is a good policy? |
Focus groups were repeated until there were no new themes emerging from the participants. Data saturation was reached by listening carefully to the conversation points, and hearing similar examples that added detail to previously noted themes. The authors consider that they were able to identify when a point of saturation was reached, with no new themes emerging.
The analysis method involved all authors individually reading hard copies of the manuscripts while using a colour-based key to identify potential themes, coming together to discuss those themes then re-reading the transcripts (electronically) to identify quotes that supported or refuted potential themes. These quotes were then noted on a separate document under the proposed theme as a heading. The authors subsequently met up to map out individual preliminary findings and to agree on areas of consensus, overlap or disagreement. The resulting map of themes, with their constituents, was transformed into a diagram (Figure 2).

Ethical approval
The aim of this work was to generate a deep understanding of relevant factors and experiences in the local context. Considering Health Research Authority (2023) guidance and because local context will vary from one institution to the next, formal ethical approval was not sought. Institutional approval was gained from the local quality improvement and safety committee (reference number 12558), and the work was approved by the deputy head of nursing for critical care on the basis that it would generate important insights into a long-standing risk register item.
Written consent from participants was not sought but, following an explanation of the work, anyone electing not to participate was given the opportunity to leave. The contact details of the pharmacists facilitating the groups were circulated so participants could follow up any concerns that emerged after the group had taken place.
Participants' names were not recorded to maintain privacy and anonymity. Transcripts were not provided to those taking part for review, primarily because of practical considerations, as the number of participants made it impractical to facilitate this.
Results and discussion
A total of 29 nurses took part in the focus groups: their demographics are described in Table 2.
Table 2. Demographics of the nurses who participated in the focus groups (n=29)
| Focus group number | Number of nurses | Male | Female | Band 5 | Band 6 | Duration of focus group |
|---|---|---|---|---|---|---|
| 1 | 7 | 2 | 5 | 5 | 2 | 17 min |
| 2 | 6 | 2 | 4 | 5 | 1 | 19 min |
| 3 | 8 | 4 | 4 | 6 | 2 | 17 min |
| 4 | 8 | 4 | 4 | 6 | 2 | 16 min |
The facilitators acknowledge that within focus groups there could be conformity bias or dominance of outspoken participants, but the use of focus groups was a pragmatic decision.
Other options such as ethnography or surveys would likely yield a small sample and there was a risk that valuable discussion points would be missed as participants would not be able to raise what they felt were important issues. The codes and themes distilled from the analysis of focus groups are detailed in Figure 2. In total, five major themes were identified: geography; IT; routine; complex process; and personnel.
Geography
Unanimously, the biggest barrier to appropriate second-checking was patients being cared for in side rooms, especially if they were isolated because of infection control measures. Comments captured various difficulties:
‘I will be banging on the [side room] window [trying to get attention from colleagues to do a second check] and people will be trying to look through the window.’
‘You tend to get everything checked even if the drugs are to be administered at bedtime, and I will prepare everything [in advance] and check with my colleague.’
These illustrate the practical problems encountered when complying with the administration policy. Checking in advance of administration does not align with local policy, but was reported to arise out of necessity. If medicines had been pre-emptively prepared, there is a potential for prescription changes to be missed if the prescription is not rechecked thoroughly at the time of actual administration.
Solutions to geographical problems associated with side rooms may be difficult, but could be considered when units are being designed or renovated. Locally, all side rooms have windows and telephones, but these rely on attracting the attention of other busy staff members in contrast to nurses working in open bays who reported facilitating second-checking by diverting or interrupting someone who happened to be passing the bedspace. Protocolising another nurse to check in regularly may still not ensure someone is there at the point of every medication administration, especially for drugs given at non-scheduled times, such as in the case of as-required medications.
IT
Participants discussed the times that medicines were default scheduled for administration on the prescribing system used locally, with morning medicines scheduled for 6am (at the end of a night shift):
‘When you have five or six IVs to give in the morning, you feel a lot of pressure to make sure you get them [done] and it's like a race against time.’
This could mean a large number of infusions to administer contemporaneously were bringing pressure, with everyone on shift looking to do the same thing at the same time, and hence fewer second checkers being available. Potentially, changing the timings or considering this issue when implementing electronic prescribing systems could improve the robustness of the second check.
A further finding was participants looking to IT to support them in executing tasks in line with trust policy. This is incongruous with the technology used in the authors' ICU; co-signing at the point of medication administration is not mandated or even prompted, and medication can be administered with only one person logged in to the medication administration system:
‘If they [the second checker] are not actively signing for it, then it does not have the gravity of the responsibility.’
The authors are not aware of any evidence that mandating a co-sign would make the second check more robust, but the act of having to log in to the IT system as the second checker may change perceptions of where the responsibility lies and, accordingly, influence behaviour.
The authors acknowledge the manner in which IT systems are set up regarding the timings of medication or mandating a second check will have a role in driving routine and, potentially, culture.
Routine
Medications that are perceived as routine within ICU may be high risk, for example opioids or electrolytes. Participants reflected a sense of it being safer to give routine medications:
‘It is a bit of a given that the patient is likely to be on five standard infusions that we give: Actrapid, fentanyl, propofol etc. Also, with your buddy when you are constantly checking their patient's stuff, you already know that they are allergic to aspirin or whatever. You tell the person I am putting up another propofol, fentanyl and they are like OK.’
There was little reflection from participants that selection errors, for example administering propofol 1% versus 2%, could have significant consequences for the patient, as described by Dickinson et al (2010). Having repetitive processes will, in most cases, result in automation; while this allows the nurse to execute the task effectively, if this is bundled with complacency or a lack of acknowledgement of the potential risks, it can be a source of risk to the patient. This was studied by Schilp et al (2014), who found adherence to double-checking was 52% for commonly used medications in Dutch hospitals.
Another consideration is whether a single, thorough check may be better at detecting errors than two potentially superficial ones:
‘If it is a single check, I would be a lot more vigilant because, if you are the only one that is signing the medication, you will make sure it is correct.’
If the responsibility lies clearly with one individual, this may cause a change in checking behaviour, whereas if two individuals are involved, each may be depending on the other to complete a full check, with the result that neither party undertakes the task completely. Koyama et al (2020), however, noted that, where double-checking policies had been implemented ‘for safety’, it would be difficult to de-implement them, despite this reflection on the gravity associated with the check reflected by this participant.
A further finding was that having a drug that required a calculation was associated with a more comprehensive second check, as there was a greater perception of risk of error at the time of administration. This finding is contrary to the research by Alsulami et al (2014), which showed only 30% compliance (591 out of 2000 events) with double-checking when administration involved a calculation.
To the authors' surprise, expiry date checks were seen as one of the most important aspects of second-checking, although this is less of an immediate priority than other pillars of second-checking, such as drug strength or diluent type. Participants described an ‘unwritten rule’ around ensuring the year was verbally checked, and both nurses agreeing the product had not expired. This appeared to be a cornerstone of the conversation that was held during double-checking:
‘You could be going somewhere with a handful of stuff and someone comes out and says can you just check this Plasmalyte, this patient has dropped their blood pressure and I go to give a bolus and you go, yeh, yeh, 2021.’
Participants reflected that commonly used drugs were felt to be familiar, perhaps recognised visually from their packaging, and potentially a lack of full scrutiny when checking these routine items presented a challenge for a member of staff performing a robust independent second check (Figure 1). It should be recognised that a degree of automaticity and system one thinking is necessary given how common medication administration is.
Complex processes
It is vital to acknowledge that nursing an intensive care patient is a dynamic, highly skilled task that can be influenced by a variety of issues from patient acuity to timing pressures and multiple competing tasks. All themes discussed above – geography, IT, routine and personnel – contribute to the complexity of nursing an ICU patient. The combination of all these with life-threatening scenarios could result in deviations from policies:
‘Nothing is prescribed in emergency – you show people the vials afterwards.’
‘Your patient is intubated, you are not going to wait and say, can someone check this rocuronium with me.’
These quotes illustrate the dynamic and stressful situations that can occur in an acute environment where the medicines policy does not capture the urgent scenarios where inaction could result in harm to the patient. This means that people are forced to work differently with regards to medication administration in general wards as the circumstances are different.
It is possible that a perception that there are ill-defined circumstances in which the medicines policy does not apply may permeate into non-emergency situations, even though the participants felt, generally, that the medicines policy was a good one. Participants reflected on having to balance processes for following safety protocols and acting swiftly, and noted the complexity this brought.
Personnel
On a critical care unit, nursing staff work together to provide care to their patients. Roles and responsibilities in providing complex care were felt to be tacitly understood and not explicitly stated. This could be a potential source of error if people have different understandings of these unwritten rules:
‘I would not question the dose too much if it is not my patient.’
The second checker felt a marginalised responsibility when conducting an independent second check. The researchers' impression was that there was a perception that the second checker was there for a type of factual accuracy check, rather than a robust, complete second check.
Experience was also felt to be a significant factor, with participants noting that more junior staff have reduced cognitive capacity (bandwidth) to undertake a robust check due to having to concentrate on non-routine tasks that require significant levels of focus:
‘Someone who is new, who is already stressed out with their workload, you will go and show them the drug and they will go, yup, yup, and you will go “do you want to check the prescription, are you happy with this?”’
It appears that junior staff feel that colleagues who are more experienced or senior may be less likely to make a mistake so they do not need to undertake a full, robust check. Overall, seniority was considered to have a strong influence on the double-checking process. Participants said that a senior member of staff is more likely to have error wisdom; they understand the risks associated with administering medication and where errors can occur:
‘This is due to their experience and being around long enough to see things go wrong.’
However, research by O'Shea et al (1999) suggested that additional education and experience had a minimal impact on medication error rates, in particular when it came to calculations (Dickinson et al, 2010).
Limitations
The focus groups were limited to 7% of all the trust's critical care nurses and the selection was a convenience sample rather than randomised. This was a site-specific piece of work conducted by novice qualitative researchers.
The use of focus groups can be limited by group and power dynamics as well as limited individual depth and social bias. In addition, some nurses were more confident and vocal than others, which could have resulted in some voices and valuable opinions not being heard and themes or lived experiences being missed.
Most trusts have different IT systems, case mixes, skill mixes of staff on shift and ward layouts, so not all the points will be relevant to all hospitals across the country. The work was intended not to be generalisable to other centres, but to contribute to understanding the local context deeply.
Conclusion
Overall, this work gives a deep explanation of local medicines administration practice in adult critical care, and the themes associated with this, including those that may prevent nurses from implementing a robust second check. This work notes instances where following the medicines policy may result in delays to patient care, so participants reported that there were times when the policy was not adhered to completely.
Mandating a second co-sign with the electronic prescribing system, where an individual would have to type in their name and password before the drug is marked as checked, could alter the psychology of checking because it may shift the balance of where the perceived responsibilities lie.
This work also supports similar findings of other studies regarding the influence of workloads, routine, complexity of the process and environmental factors on preventing a consistent robust second check.
Overall, ethnographic studies are required at ward level as a bigger piece of work to further understand second-checking. This work could include capturing how often second-checking picks up error, challenging whether a second check is effective in improving patient safety, or whether there is a place for a single check of certain medications within the current NHS climate. Further studies could also explore the use of technologies such as barcoded medication administration systems.
KEY POINTS
- Independent second-checking of medication is part of everyday practice in the NHS to prevent drug errors
- To prevent medication errors, independent second-checking policies are in place in many NHS hospitals
- These policies set out the steps involved in administering and checking medications, and assume that there are no problems regarding the resources to do so, including personnel and time constraints
- Five themes were associated with barriers and enablers to second checking: geography, IT, routine, complex process and personnel
- Side rooms are a major barrier to a robust second check
- Where a parenteral medicine requires a calculation step or where there was a degree of unfamiliarity with the drug, a more robust second check was reported
CPD reflective questions
- What barriers do you perceive to performing a robust independent second check of medication?
- How could you optimise your checking process to improve patient safety?
- What drawbacks do you see with having a single check for certain medicines within intensive care units? Do you think a single check of intravenous medication before administration would be superior, inferior or the same in terms of preventing harm to patients from medication errors compared to a double check?
- Do you feel that your practice as a first checker is different to your practice as a second checker?


