References
Prevalence of post-traumatic stress disorder and its predictors following coronary artery bypass graft surgery
Abstract
Background:
Cardiac surgery can be traumatic and stressful, and as a result many people experience psychological difficulties following treatment.
Aim:
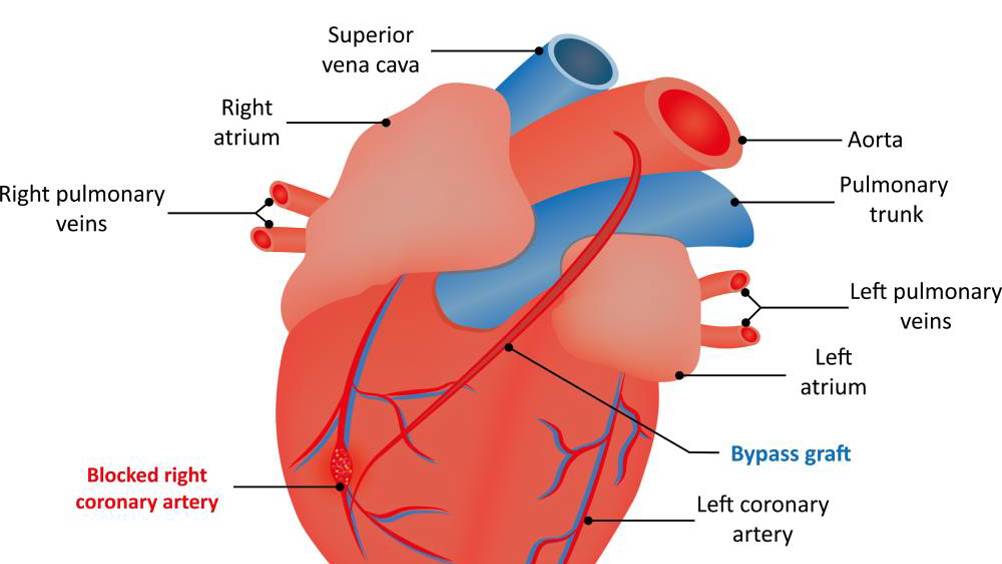
To assess the level of post-traumatic stress disorder (PTSD) 1 month after coronary artery bypass graft (CABG) surgery among Jordanian patients, and to examine the predictors of PTSD after 1 month.
Method:
A descriptive survey design was used.
Findings:
149 patients participated in the study. Their mean age was 59 years (SD=10.2) and most were male (87%) and married (93%). Some 44% of patients had PTSD. Length of stay in hospital (c² (1)=6.598, P<0.05), and age (c² (1)=4.920, P<0.05), predicted the occurrence of PTSD after 1 month.
Conclusions:
Nurses, who are usually in the frontline with patients, should consider using a robust tool and clinical interview to assess and evaluate the presence and the risks of PTSD to promote early detection and optimal management. Follow-up studies after 6 and 12 months would be beneficial.
Post-traumatic stress disorder (PTSD) is a complex condition that results from exposure to a traumatic events (American Psychiatric Association (APA), 2013). According to the Diagnostic and Statistical Manual of Mental Disorders(DSM-5) (APA, 2013), a diagnosis of PTSD is made when the symptoms persist for more than 1 month after the traumatic event. These events include, but are not limited to, armed struggle, physical assault, sexual violence, kidnapping, terror attacks, torture, natural or man-made disasters, motor vehicle accidents or life-threatening illness. Having a life-threatening illness might not necessarily be considered a traumatic event, although incidents related to the illness, which may be sudden or tragic, can be triggered by it (APA, 2013).
Individuals with PTSD experience several distressing symptoms, classified into three categories: re-experiencing symptoms such as intrusive thoughts, nightmares or flashbacks; avoiding stimuli or reminders of the event; and physiological arousal (for example, hypervigilance, exaggerated startle response) (APA, 2013). Sensory disturbances can be distressing and have been associated with prolonged psychological distress and heightened physiological arousal (Kok et al, 2016). Individuals with PTSD often limit their social interactions, affecting their quality of life and psychosocial outcomes (APA, 2013). They may also experience reduced interest in usual activities and persistent anhedonia, and engage in irresponsible behaviours such as drug use or excessive alcohol consumption (APA, 2013). Further disability is seen in social and family relationships, work attendance, income status, occupational success, education levels and general quality of life (Hauer et al, 2013).
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
-
Limited access to clinical or professional articles
-
Unlimited access to the latest news, blogs and video content

