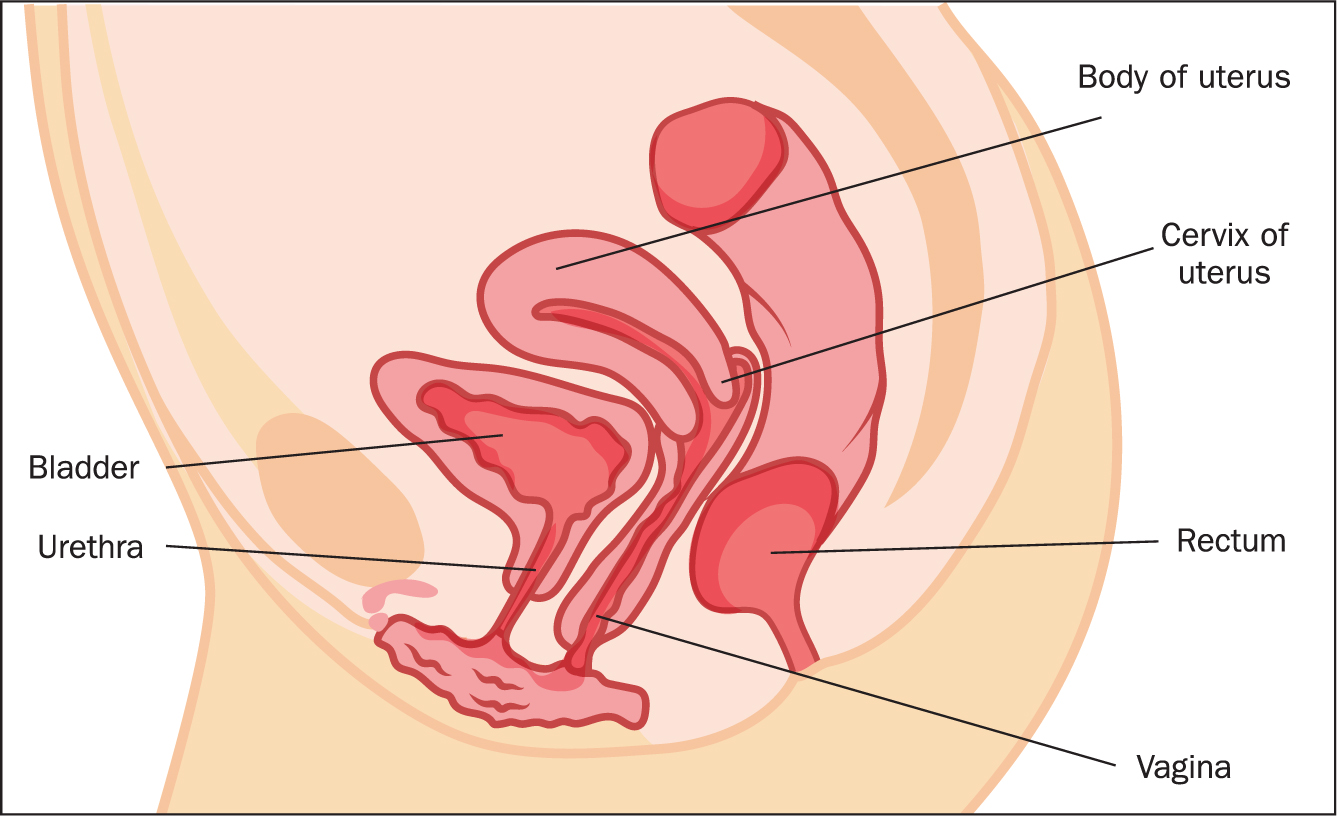
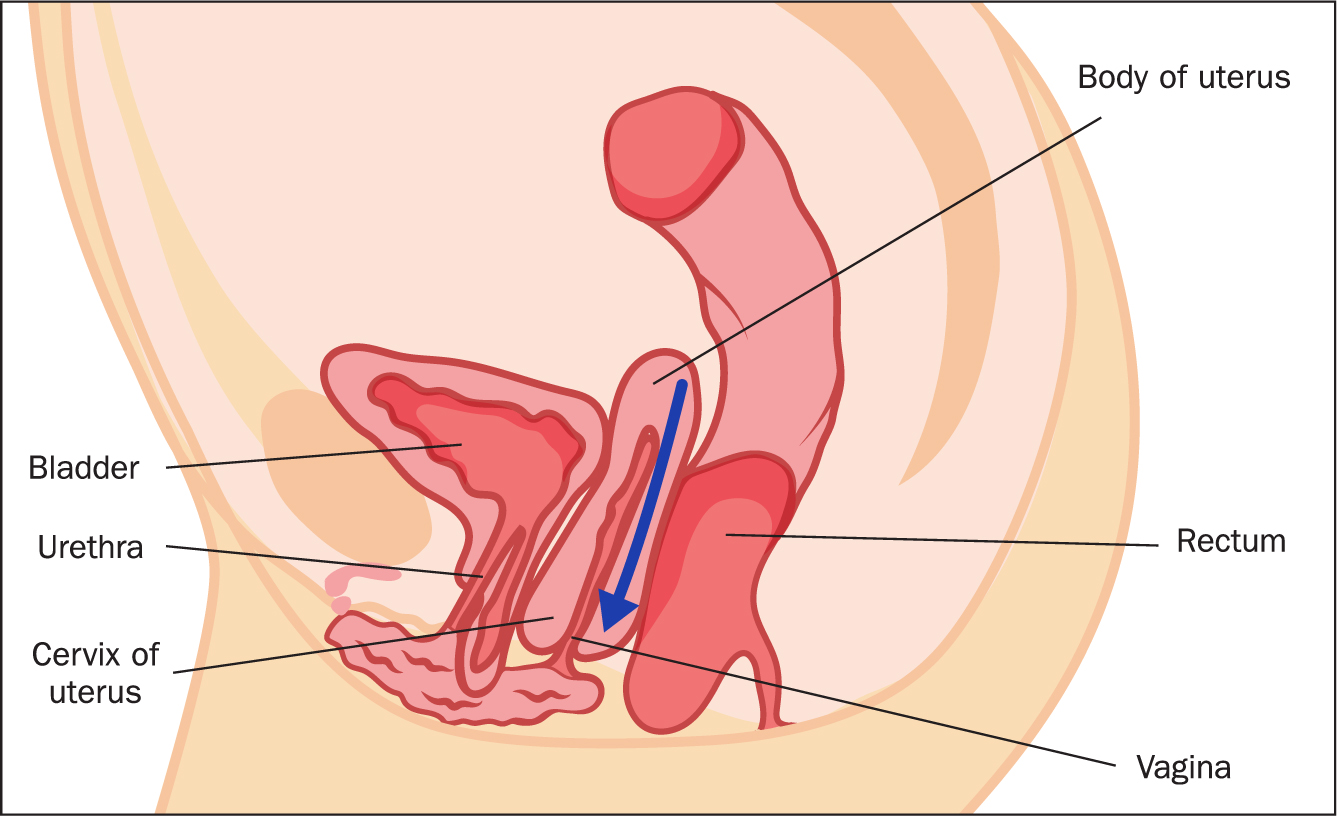
Prolapse of the pelvic organs occurs when the hammock-like pelvic floor muscles extending from the pubic bone to the coccyx or the levator ani muscles that hold the pelvic floor closed become weak or injured and fail to support one or more of the pelvic organs, namely the bladder, uterus or rectum, causing them to protrude outside the body in advanced cases (see Figure 1 showing a normal uterus and Figure 2 showing a prolapse, stage 3, as described in the case study).
Although not life-threatening, pelvic-organ prolapse can be life limiting and adversely affect physiological processes, function and quality of life, with those affected reporting years of pain, discomfort, humiliation and embarrassment (Ramage et al, 2022).
Under-reporting of uterine prolapse may be attributed to women feeling resigned to a condition that is often dismissed as part of getting old, the menopause or a consequence of childbirth. Additionally, anecdotal evidence indicates that reluctance to seek help may arise from embarrassment because of stigma or a fear of becoming the object of ill-considered jokes.
This article focuses on uterine prolapse, management of symptoms including conservative self-help and, in advanced stages, surgical options. A case study describes a safe and successful procedure undertaken by a skilled surgeon using bifurcated polypropylene mesh.
Prevalence
The prevalence of uterine prolapse varies, depending on reporting methods and assessment categorisation, and may be more common than is realised. Uterine prolapse was found in 14% of women in a US study of 27 342 women (Doshani et al, 2007) and, in the UK, it is estimated that 50% of parous women have some degree of prolapse, of whom only 10-20% will seek medical care.
According to Thakar and Stanton (2002), women with genital prolapse accounted for 20% of the waiting list for major gynaecological surgery. Recently, the Royal College of Obstetricians and Gynaecologists (RCOG) (2022) revealed that gynaecology, the only specialty that caters for women, seemed to have the fastest growing waiting lists, with more than 570 000 women across the UK waiting for care. The RCOG (2022) report found that this was more than 60% higher than before the COVID-19 pandemic, with the number of women waiting for an appointment for more than a year in England rising from 66 before the pandemic to nearly 25 000 after.
Delays in care have resulted in increased costs for both the NHS and women, with a service that ‘seemed to bear the brunt of cuts’ when pressure was put on the NHS during the COVID-19 pandemic (RCOG, 2022).
Studies have identified the condition in young as well as older women, occurring in those aged 19–71 years (Leron and Stanton, 2001; Price et al, 2010).
Epidemiological data are unreliable because of under-reporting, with women ‘getting on with it’ and having a reduced quality of life or being unaware of the options and/or self-help remedies to prevent the condition deteriorating or alleviate symptoms.
Risk factors
There are a number of risk factors for the condition:
- Predisposing genetic factors such as low oestrogen levels or weak pelvic floor muscles
- Pelvic or abdominal congestion caused by disease
- Prolonged and persistent coughing bouts
- History of constipation
- Obesity
- Smoking
- Multiparity, particularly difficult vaginal births
- Lifestyle, eg lifting and/or carrying heavy weights
- Stress.
Signs and symptoms
Not all women will experience all of the symptoms listed here, which will vary according to the degree of prolapse. As the uterus becomes displaced in the early stages, symptoms may not always be obvious or troublesome, with the condition remaining undetected and gradually deteriorating. Symptoms include:
- A feeling of heaviness and ‘something coming down’
- Pain and or discomfort in the pelvis
- Urgency of micturition, with incontinence in some cases
- In first- and second-degree prolapse, an obvious bulge that may or may not be possible to push back into place
- A feeling of ‘everything being open’
- Sexual activity problems.
Possible consequences of poor or no management
A lack of proper attention to the problem can cause the following:
- Urinary problems: the bladder is sometimes called an ‘emotional organ’ as problems can be exacerbated by stress
- Bowel-emptying problems because of localised pressure
- Sexual problems with changes in anatomy
- Problems with getting pregnant or during pregnancy
- Inability to lift normal-weight objects or walk for long distances.
In addition, there can be social and psychological consequences, including:
- Embarrassment and anxiety about symptoms
- Isolating from others and a reluctance to socialise, leading to restricted mobility
- Hopelessness about the condition and how it is perceived and managed.
Challenges for management
Compounding the problem are long waiting lists for the referral and treatment of conditions classed as non-urgent, with gynaecology being the worst affected (RCOG, 2022). According to the RCOG report, of 180 000 women waiting for longer than 18 weeks from referral to treatment in gynaecology in England, 40% had been waiting for longer, which is higher than the average for all specialties (under the NHS, 18 weeks should be the maximum wait for non-urgent cases).
Many women are reluctant to seek help and, when they do, they are not always offered solutions that are acceptable to them. Options for mild prolapse include pelvic floor exercises and oestrogen cream and, for more advanced prolapse, ring pessaries to hold everything in place. However, this last option as reported in one study was not always acceptable to patients, who can perceive it as ‘another level to my life that I just can't handle’ (Ramage et al, 2022).
Surgical options include hysterectomy, the most commonly performed procedure for the condition, but it may not be suitable for all patients, particularly those who are too ill for major surgery, or women who may wish to bear children. A Turkish study found that uterus-sparing surgery such as sacrohysteropexy did not disturb the pelvic anatomy, thereby preserving women's self-esteem and sexuality. Additionally, bleeding and longer operating times were less likely (Tola et al, 2015).
Similarly, Price et al (2010), in a 51-patient study in the UK, identified restoration of the vagina and a favourable functional outcome following laparoscopic hysteropexy. The use of mesh is controversial, however, because inappropriately placed mesh can become fused with adjacent tissue (Devlin, 2017). Techniques have been developed to overcome this problem by using the mesh in a different way (Leron and Stanton, 2001; Price et al, 2010).
Case study
Mrs A a fit, slim, active and otherwise healthy woman in her sixties, first sought help from her GP when her symptoms had progressed to the third degree and she felt she could no longer manage the condition herself.
Mrs A's medical history did not include the usual risk factors except for a prolonged period of lifting and carrying heavy objects for her work in her later years and a short spell exercising at the gym, including squats and weightlifting. She was not overweight and had given birth to two healthy babies, both of normal weight and full term, with uneventful pregnancies and short-duration, uncomplicated vaginal births. Menstruation had been regular and not unduly heavy, and a relatively easy menopause had followed.
She was referred by her GP to the specialist physiotherapy team, who advised on diet to manage bladder irritability and started her on a pelvic floor exercise programme aided by the NHS Squeezy App to aid compliance. However, despite conscientious lifestyle changes of correct diet, not walking for too long, not lifting weights and doing her exercises regularly as instructed, Mrs A's condition appeared to deteriorate.
At her insistence, she was referred to a gynaecologist who offered three solutions: insertion of a ring pessary; topical oestrogen cream; or a hysterectomy. Considering these options, Mrs A was adamant that a ring pessary was not for her and she was reluctant to have a hysterectomy, which she believed would not resolve the problem without recurrent prolapses of other organs in the future. She agreed to try the oestrogen cream but that did not improve the condition, although it did make her feel more comfortable locally.
Following a few small bleeds per vagina, in-depth examinations and hysteroscopies were performed on two separate occasions, both of which excluded cancer. She continued to attend the physiotherapy clinic and, although the physiotherapist was helpful, encouraging and sympathetic, she admitted that exercises alone would not fix the condition given its advanced stage.
By this time, the pandemic had struck and life was made even more uncomfortable by the lack of public toilets that were open during the first lockdown, leading to further isolation as Mrs A refused to go on long-distance walks with friends, preferring to walk alone for a few minutes around the block, returning home to use the toilet, and going out again. The cold seemed to exacerbate her symptoms and she devised several clothing ensembles to keep everything in place and warm, without placing undue pressure on her abdomen with tight waistbands.
Believing that the problem would never be resolved because of the pressures on the NHS, Mrs A decided to seek a private solution. After considerable research, she saw a consultant gynaecologist who specialised in a new procedure involving a laparoscopic hysteropexy with polypropylene mesh apical support. The surgeon explained how this procedure overcame the problems of the old method of vaginal mesh repair that had led to complications in the past. In women who still have a uterus, the mesh is placed around the cervix and is kept away from the vagina, preventing problems such as vaginal mesh erosion.
The specialist centre had published its results after 10 years in a follow-up study of 507 patients who had undergone this procedure, with 93.8% expressing very much or much better success and satisfaction, with a complication rate of 1.8% and 2.8% of patients needing repeat apical surgery (Jefferis et al, 2017). Although it was a complex operation under general anaesthetic, Mrs A was in hospital for two nights and was discharged once she was able to pass urine and mobilise. Postoperatively, she experienced constipation for about one week and some degree of back pain that was relieved with mild analgesia.
Recovery was shorter and less complicated than it would have been following a hysterectomy and the small scars from the puncture sites are now almost imperceptible.
Discussion
Although guidance advocates conservative management of uterine prolapse with pelvic floor exercise programmes and a ring pessary (National Institute of Health and Care Excellence (NICE), 2009), these may not be options for all patients, particularly those at advanced stages. Costs of management should not be the only criteria as patients deserve the best quality of life and long-term outcomes. However, solutions that provide these may not always be recommended by the health service.
Concerns relating to the use of mesh for hysteropexy are based on older evidence, traditional practice and not having the resources or specialist surgeons who are skilled and experienced in new procedures. Many health professionals and the general public have expressed fear about the use of mesh, which has been associated with inappropriate procedures resulting in the mesh becoming integrated into the soft tissues in the body and becoming difficult to remove. This has led to NHS (2009) guidance advising caution on its use.
On the other hand, hysterectomies may have been performed as an excessive measure with consequences of denied childbearing or, in some cases, further loss of support in the vaginal vault, leading to risks of further prolapses (Dietz et al, 2009). Additional complications of invasive surgery include the risks of infection, bleeding and scarring as well as deep-vein thrombosis, which is associated with long recovery and sustained immobility.
In the right hands, laparoscopic hysteropexy with apical support can be a safe, effective alternative to hysterectomy (Jefferis et al, 2017; Nightingale and Phillips, 2021), and this was certainly a better option for Mrs A, who made a speedy, uneventful recovery, followed by a return to her former state of health and wellbeing.
Mrs A continues to perform her pelvic floor exercises and is careful about lifting and carrying heavy weights when shopping or during rigorous gym workouts. It has lifted her spirits to be able to wear normal clothing, go for walks without frequent toilet breaks, and to feel healthy and feminine again.
Unlike many chronic conditions, uterine prolapse is not visible, being mostly hidden from others by those affected. The low priority allocated for its treatment or mismanagement by healthcare providers have resulted in long waiting lists and, in some cases, years of feeling isolated and enduring pain. Many women have been denied the opportunity to have children and older women have lost their independence because they fear leaving the house because they need reassurance that a toilet is nearby.
Advice for women with a uterine prolapse is given in Box 1. Websites containing useful information for practitioners and women are listed in Box 2.
Box 1.Advice for women with uterine prolapse
- Avoid heavy lifting or carrying
- Take care in the gym when doing squats and lifting weights
- Upper-body exercises using weights can be performed while lying down or seated
- Follow a sensible diet and watch your weight
- Avoid becoming constipated and keep hydrated
- Stop smoking
- Avoid carrying heavy bags while walking
- Try not to sit for long periods
- Keep doing your pelvic floor exercises
- Seek help from family, friends and professionals if you are worried. Avoid feeling stressed
- Explore all the management options and choose the one that is right for you
Box 2.Online resources for practitioners and womenThe following links provide information for practitioners involved in surgical procedures using mesh and provide information for patients who need to make informed decisions about their treatments:
- National Institute for Health and Care Excellence. Surgery for uterine prolapse. Patient decision aid 2019. https://tinyurl.com/5n6e8hsk
- National Institute for Health and Care Excellence. Surgery for uterine prolapse Patient decision aid: user guide and data sources. 2019. https://tinyurl.com/32h4puss
- National Institute for Health and Care Excellence. Urinary incontinence and pelvic organ prolapse in women: management. 2019. https://www.nice.org.uk/ng123
- Oxford University Hospitals NHS Foundation Trust. Laparoscopic hysteropexy. Information for women. 2020. https://tinyurl.com/2p89m23c
- Royal College of Obstetricians and Gynaecologists, British Society of Urogynaecology. Post-hysterectomy vaginal vault prolapse. 2015. https://tinyurl.com/ypx97avs
Conclusion
Many women are still tolerating prolapse in silence because of low awareness of a condition that can be addressed and resolved with treatments available on the NHS. This could improve their wellbeing and confidence, the future functioning of all pelvic organs and their lives in general.
Mrs A was fortunate to be able to bypass NHS waiting list and afford appropriate treatment, in this case private surgery, after making an informed decision because she was made aware of all the risks, benefits and options.
The skills of a good surgeon who is prepared to adopt the latest, evidence-based techniques and the experience of senior physiotherapists should not be underestimated.
Most of all, successful management of this treatable condition depends on practitioners understanding patients and their willingness to take responsibility for a patient's lifelong care and management.
KEY POINTS
- Gynaecology has the longest waiting lists of all specialties for treatment
- Incidence of uterine prolapse is underestimated and management of the condition is underfunded
- The condition is under-reported because of a lack of awareness, embarrassment or simply resignation
- Although not life threatening, uterine prolapse can have a significant impact on physical, mental, emotional and sexual health
- Options are not always acceptable to patients or, in the case of mesh supports, not offered because they are controversial
CPD reflective questions
- What advice would you give to patients who may be at risk and who may have early symptoms?
- How would you raise awareness of the condition, and encourage patients, colleagues and the general public to be more open about discussing the condition?
- When would you recommend that a patient is referred for specialist opinion or surgery?
- How can you ensure that patients are aware of all available options, as well as the risks and benefits, including uterus-sparing surgery, to help them make an informed choice?


